Top videos

How to perform a parotidectomy gland resection? In this video we take you step by step through the protid gland resection surgical technique. This video is intended for ENT residents and Head and Neck Surgery Surgeons. It is part of the ORL-Information's Head and Neck surgery Masterclass in collaboration with the University Hospital of Nîmes. Surgeons Editors: Pr. Benjamin LALLEMANT, MD, PhD - Dr. Camille GALY, MD Head and and Neck Department, University Hospital of Nîmes, France Official video | www.orl-information.fr
Cette vidéo présentent la technique de la parotidectomie avec dissection du nerf facial. Elle illustre les différents temps de l'intervention notamment le temps de repérage du nerf facial.
--------------------------------------
@Prévention médecine | Comment préserver sa santé ?
✔Abonnez-vous à la chaîne ORL-Information : https://www.youtube.com/c/ORLINFORMATION
✔Retrouvez-nous sur internet: https://www.orl-information.fr
Cluster headaches, which occur in cyclical patterns or clusters, are one of the most painful types of headache. A cluster headache commonly awakens you in the middle of the night with intense pain in or around one eye on one side of your head. Bouts of frequent attacks, known as cluster periods, can last from weeks to months, usually followed by remission periods when the headaches stop. During remission, no headaches occur for months and sometimes even years. Fortunately, cluster headache is rare and not life-threatening. Treatments can make cluster headache attacks shorter and less severe. In addition, medications can reduce the number of cluster headaches.

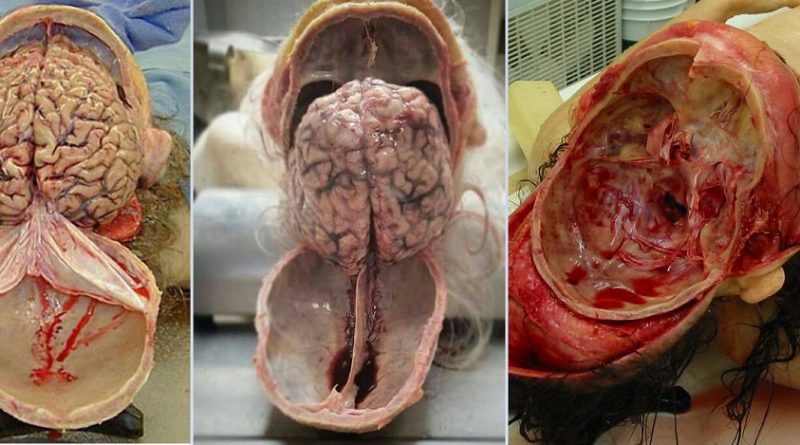
Doctors save the life of an unborn baby who was injured along with her mother in a missile attack in the Syrian city of Aleppo. The video shows a team of emergency medical workers delivering the baby by Cesarean section and then treating the newborn for the shrapnel wounds covering her body and one very large gash in her head. “Medics can be seen frantically reviving the baby, after delivering her by emergency cesarean, as she lies motionless,” the article states. “Eventually the tiny newborn begins to cry and seemingly comes to life as she is given an oxygen mask and rubbed vigorously.” “According to Reuters, the woman also has three other children, all of whom were injured in the attack, but are reported by doctors in the hospital to be in a good condition,” the Daily Mirror article states. The article does not provide the gestational age of the baby before it was delivered. The article said the pregnant woman was hit by a barrel bomb – “crude explosives and shrapnel and dropped from helicopters used by [Syrian] President Bashir al-Assad’s regime." The article notes an estimated 7.6 million Syrians have been displaced by the ongoing civil war and that 320,000, including 11,000 children, have been killed in the conflict. The Daily Mirror also reports that the doctors suggested that the tiny girl be named Amal, which means hope in Arabic. UK Daily Mirror: Incredible footage shows Syrian doctors perform lifesaving caesarean after missile strike leaves shrapnel embedded in unborn baby's face
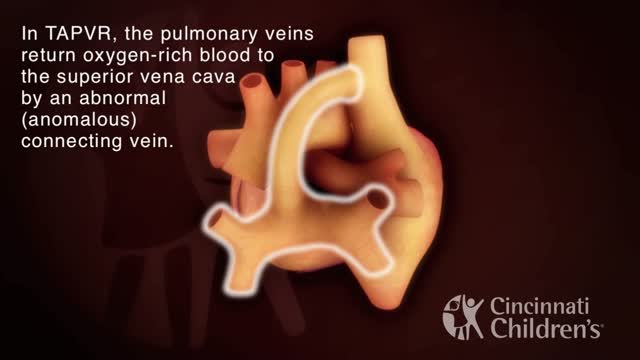
Total anomalous pulmonary venous return (TAPVR) is a rare congenital malformation in which pulmonary veins that return oxygen-rich blood from the lungs do not connect normally to the left atrium. Instead all four pulmonary veins drain abnormally to the right atrium. Heart models and animation were developed by the Cincinnati Children's Heart Institute in conjunction with Cincinnati Children's Critical Care Media Lab.

Marfan syndrome is a genetic disorder that affects the body's connective tissue. Connective tissue holds all the body's cells, organs and tissue together. It also plays an important role in helping the body grow and develop properly. Connective tissue is made up of proteins.

The baby suffered from ectopia cordis, a rare condition where a baby's heart is located either partially or totally outside the chest. Only 8 out of 1 million babies are born with the condition, and 90 percent of those babies are either stillborn or die within the first three days of life.

Septic arthritis is also known as infectious arthritis, and is usually caused by bacteria, or fungus. The condition is an inflammation of a joint that's caused by infection. Typically, septic arthritis affects one large joint in the body, such as the knee or hip. Less frequently, septic arthritis can affect multiple joints
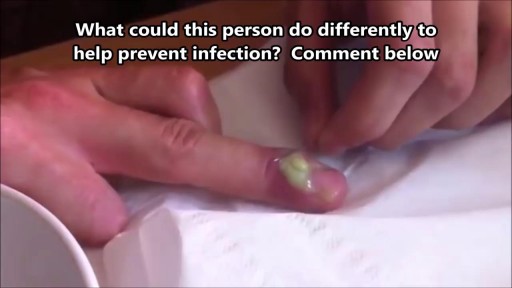
What Is a Paronychia (Nail Infection)? An infection that develops along the edge of the fingernail or toenail is called a paronychia (pear-ah-NIK-ee-ah). It is the most common hand infection and, if left untreated, can progress to a more severe infection of the entire finger or toe. Paronychia is distinguished from other infections such as onychomycosis and herpetic whitlow by its location and appearance.

A lot of women want to know what type of vaginal discharge is normal during pregnancy, and when you're not pregnant. So let's start out by talking about what's normal when you're not pregnant. It's normal to have about 1/2 teaspoon to 1 teaspoon of whitish, creamy, tannish discharge on most days of your cycle in between periods, with the exception of the time of ovulation. Actually, around the time of ovulation, it's normal to notice the discharge becoming more slippery and clear, almost like egg whites. And this is actually a sign that you can watch for to know when you're ovulating. And if you're seeing this type of discharge and you're trying to have a baby, then you should start to time intercourse with ovulation to increase your chances of conceiving.
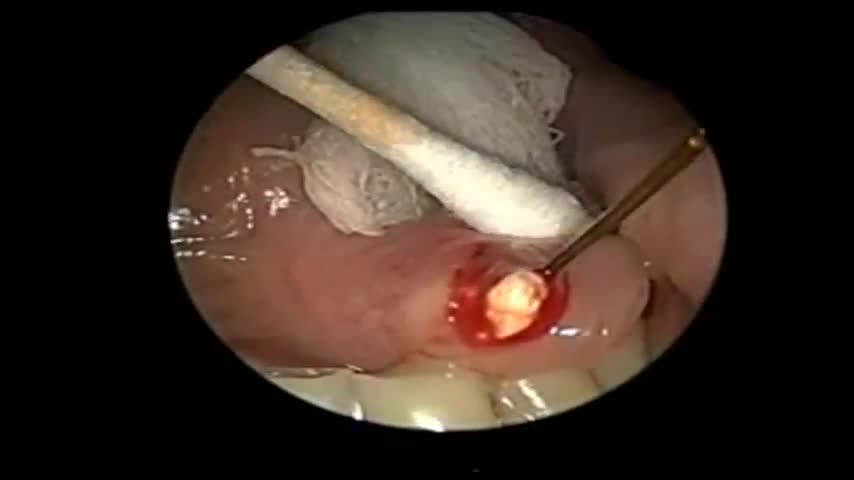
Sialendoscopy can be both diagnostic and therapeutic. It is complementary to diagnostic techniques such as plain radiography, ultrasonography, computed tomography (CT), magnetic resonance sialography, and conventional sialography, all of which are traditional, time-tested methods for evaluating the salivary ductal system

Ingrown toenails occur in both men and women. According to the National Health Services (NHS), ingrown toenails may be more common in people with sweaty feet, such as teenagers. Older people may also be at higher risk because toenails thicken with age. Many things can cause an ingrown toenail, including: cutting toenails incorrectly (Cut straight across, since angling the sides of the nail can encourage the nail to grow into the skin.) irregular, curved toenails footwear that places a lot of pressure on the big toes, such as socks and stockings that are too tight or shoes that are too tight, narrow, or flat for your feet toenail injury, including stubbing your toe, dropping something heavy on your foot, or kicking a ball repeatedly poor posture improper foot hygiene, such as not keeping your feet clean or dry genetic predisposition