Top videos

Fibroadenomas (fy-broe-ad-uh-NO-muhz) are solid, noncancerous breast tumors that occur most often in adolescent girls and women under the age of 30. You might describe a fibroadenoma as firm, smooth, rubbery or hard with a well-defined shape. Usually painless, a fibroadenoma might feel like a marble in your breast, moving easily under your skin when touched. Fibroadenomas vary in size, and they can get bigger or even shrink on their own. Fibroadenomas are among the most common breast lumps in young women. Treatment may include monitoring to detect changes in the size or feel of the fibroadenoma, a biopsy to evaluate the lump, or surgery to remove it.

As a pediatric surgeon at NewYork-Presbyterian/Weill Cornell Medical Center, Dr. Nitsana Spigland treats newborns, children, teens, and young adults requiring surgical interventions. She specializes in antenatal counseling and newborn congenital malformations.
Learn more about Dr. Spigland at: https://www.nyp.org/physician/nspigland.

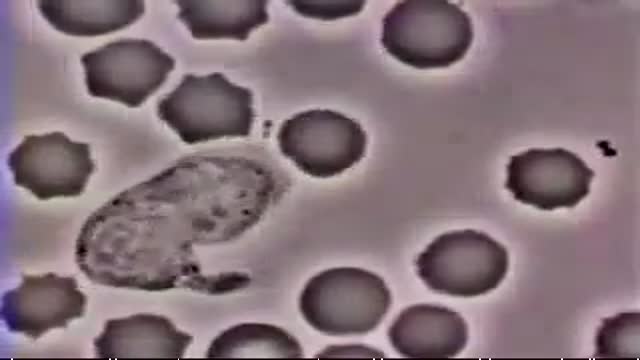
An animation of blood flow inside the hollow fiber of a hemofilter, or a dialyzer, and the flow of the dialysate in an opposite direction with increased extraction of waste and small molecules from the blood as the concentration of these molecules is reduced downstream and exposed to new dialysate.
To learn about Hemodialysis..
https://www.thevirtualnephrolo....gist.com/specialties
The Virtual Nephrologist is your gateway to optimal health.
To learn more about Hypertension, Kidney Disease and Dialysis:
https://thevirtualnephrologist.com/
About Dr. Rifai:
Dr. Ahmad Oussama Rifai is certified by the American Board of Internal Medicine (ABIM) in the specialty of Internal Medicine and the sub-specialty of Nephrology.
MEET DR. RIFAI
https://www.thevirtualnephrologist.com/rifai/
Follow The Virtual Nephrologist on SOCIAL MEDIA:
-Facebook: https://www.facebook.com/thevirtualnephrologist
-Instagram: https://www.instagram.com/thevirtualnephrologist/
-Twitter: https://twitter.com/VNephrologist
-TikTok: https://www.tiktok.com/@thevirtualnephrologist
Schedule a virtual consult:
https://www.thevirtualnephrolo....gist.com/schedule-a-
Best wishes for great health | The Virtual Nephrologist

The cause for TS is unknown. Early research suggested that TS is an inherited condition (often, the person's near or distant relatives have had some form of transient or chronic tic disorder or associated symptoms). Recent studies point to a combination of environmental and genetic factors as a cause of the disorder. The specific genes involved in the development of TS are still being investigated. Studies suggest that TS has a neurological basis and results from an abnormality which affects the brain's metabolism of certain neurotransmitters (chemicals in the brain that regulate behavior.) Current research being funded by the Tourette Syndrome Association (TSA) will help provide more information about the causes and genetic factors of TS.

Step in the Clinic with Dr. Pritesh Singh and get a practical insight into the Clinical Examination of Incisional Hernia.
Now Save Time with these Exam Relevant Clinical Videos & Waste None Studying Rare Cases.
Prepare with 2021 Dream Pack. It includes everything you need to ace Medical PG Entrance Exams. To enroll or know more visit: https://premium.prepladder.com/
=======================================================
To experience PrepLadder's excellent learning, download the app:
iOS: https://bit.ly/prepladderios
Android: https://bit.ly/prepladderandroid
Follow us on Social Media for all the latest updates:
Facebook: https://www.facebook.com/medic....al.pg.entrance.prepl
Instagram: https://www.instagram.com/prepladder_med
Subscribe to our YouTube channel and press the bell icon for more videos and regular updates: https://www.youtube.com/channe....l/UCdbMxSVAgPENqhYVe
#PrepLadder #ClinicalEssentials #PadhoWoChahiyeJo #DrPriteshSingh #Surgery #NEETPG #IncisionalHernia #2021DreamPack
Absence seizures involve brief, sudden lapses of consciousness. They're more common in children than adults. Someone having an absence seizure may look like he or she is staring into space for a few seconds. This type of seizure usually doesn't lead to physical injury. Absence seizures usually can be controlled with anti-seizure medications. Some children who have them also develop other seizures. Many children outgrow absence seizures in their teens.

Although it demands an advanced set of skills that remain substantially hard to do, many of the salient steps of “open” surgery, including suturing, are credibly “replicated” in its laparoscopic counterpart with the intention of achieving similar optimal results. This video demonstrates how to tie Laparoscopic Roeder's Knot. Laparoscopic Roeder's Knot is one of the oldest knots used in laparoscopic surgery. It is used most commonly during laparoscopic appendectomy surgery. Recent literature, though abundant with numerous reports pertaining to a variety of endoscopic knotting techniques and technologies, appears to lack scientific data but Roeder's knot is a time tasted extracorporeal slip knot that is secure for 6-8 mm diameter tubular structure.
For more information please contact:
World Laparoscopy Hospital
Cyber City, Gurugram, NCR DELHI
INDIA 122002
Phone & WhatsApp: +919811416838, + 91 9999677788

https://bit.ly/3HIStRc #shorts
Tracheotomy and tracheostomy are surgical procedures that create an opening in the trachea (windpipe) to help patients breathe when they have difficulty doing so through the nose or mouth. Though they are similar in purpose, there are some key differences between them.
Tracheotomy is a temporary procedure that involves creating a small incision in the trachea to insert a breathing tube. The tube is typically removed once the patient no longer requires it, and the incision heals on its own. Tracheostomy, on the other hand, is a more permanent solution that involves creating a hole in the trachea and inserting a tracheostomy tube, which remains in place for an extended period.
Indications for these procedures include:
Airway obstruction due to trauma, tumors, or infection
Severe respiratory distress or failure
Prolonged mechanical ventilation
Inability to protect the airway due to neurological disorders or impaired consciousness
Steps for performing a tracheotomy and tracheostomy:
Preparation: The patient is positioned, and the neck area is cleaned and draped. Local anesthesia is often administered, although general anesthesia may be used in some cases.
Incision: A small incision is made in the neck, and the muscles and tissues are carefully separated to expose the trachea.
Tracheal opening: A small opening is made in the trachea, typically between the second and third tracheal rings.
Tube insertion: A tracheotomy tube is inserted through the incision and into the trachea for a tracheotomy, while a tracheostomy tube is inserted for a tracheostomy. Both tubes are secured in place.
Confirmation: Proper placement of the tube is confirmed by listening for breath sounds and checking for adequate ventilation.
Pre-operative care typically involves a thorough assessment of the patient's medical history, as well as any necessary imaging studies or lab tests to ensure the procedure is appropriate and safe. Informed consent should be obtained from the patient or their legal representative.
Post-operative care includes monitoring the patient's vital signs, ensuring the tube remains secure and patent, and managing any pain or discomfort. For tracheostomy patients, regular cleaning and maintenance of the stoma (the opening in the trachea) and the tracheostomy tube are essential to prevent infection and other complications. Long-term care may involve speech therapy, respiratory therapy, and support from a multidisciplinary team to address any ongoing needs.
It's crucial to remember that these procedures should only be performed by trained medical professionals in a clinical setting.
for additional information about this procedure check our article @ www.medicalartsshop.com
For more free resources, find us on Pinterest & Facebook pages:
https://www.pinterest.ca/medicalartsofficial/
https://www.facebook.com/Medicalartsofficial
https://www.youtube.com/@medic....alarts?sub_confirmat
https://www.instagram.com/medicalartsofficial/
https://www.tiktok.com/@medicalarts
This video and associated content are for entertainment and educational purposes only!!

Doctors save the life of an unborn baby who was injured along with her mother in a missile attack in the Syrian city of Aleppo. The video shows a team of emergency medical workers delivering the baby by Cesarean section and then treating the newborn for the shrapnel wounds covering her body and one very large gash in her head. “Medics can be seen frantically reviving the baby, after delivering her by emergency cesarean, as she lies motionless,” the article states. “Eventually the tiny newborn begins to cry and seemingly comes to life as she is given an oxygen mask and rubbed vigorously.” “According to Reuters, the woman also has three other children, all of whom were injured in the attack, but are reported by doctors in the hospital to be in a good condition,” the Daily Mirror article states. The article does not provide the gestational age of the baby before it was delivered. The article said the pregnant woman was hit by a barrel bomb – “crude explosives and shrapnel and dropped from helicopters used by [Syrian] President Bashir al-Assad’s regime." The article notes an estimated 7.6 million Syrians have been displaced by the ongoing civil war and that 320,000, including 11,000 children, have been killed in the conflict. The Daily Mirror also reports that the doctors suggested that the tiny girl be named Amal, which means hope in Arabic. UK Daily Mirror: Incredible footage shows Syrian doctors perform lifesaving caesarean after missile strike leaves shrapnel embedded in unborn baby's face

This 35 years old man lost his right wrist in metal lathe cut machine. the video is taken about 2 years after replantation. You can see another videos in my site: https://drliaghatclinic.com, https://instagram.com/liaghatclinic, https://t.me/liaghatclinic

You can now test your knowledge with a free lesson quiz on NURSING.com!
Click here for your free quiz: https://bit.ly/3GF9I3h
NG (Nasogastric) Tube Insertion Techniques (Nursing Skills)
FREE Nursing School Cheat Sheets at: http://www.NURSING.com
Get the full lesson on NG Tube Insertion here:
https://nursing.com/lesson/ski....lls-04-01-inserting-
Get Access to Thousands of Lessons here:
https://nursing.com/courses/
Welcome to the NURSING Family, we call it the most supportive nursing cohort on the planet.
At NURSING.com, we want to help you remove the stress and overwhelm of nursing school so that you can focus on becoming an amazing nurse.
Check out our freebies and learn more at: (http://www.nursing.com)
NG (Nasogastric) Tube Insertion Techniques (Nursing Skills)
In this video we’re going to show you the correct technique for insertion of an NG tube or Nasogastric tube). We’ll also give you a few tips and tricks we use. Of course, before you get started, make sure you’ve determined which nare is more patent and that the patient doesn’t have a deviated septum. Before you start, lay a towel across the patient’s chest – I’m telling you I’ve had patients throw up on me – this step is WORTH IT!! We love you guys! Go out and be your best selves today! And, as always, happy nursing!
Bookmarks:
0.05 Introduction to NG Tube Insertion techniques
0.25 Towel placement
0.32 Measuring NG tube length
1.04 Tape preparation
1.27 Give patient water
1.34 NG Tube lubrication
1.42 NG Tube insertion technique
2.25 Securing the NG tube
2.36 Checking placement/ aspiration
2.55 Assessing pH
3.08 Confirming placement
3.22 Waiting for abdominal X-ray
3.35 Supply clean-up
3.48 NG Tube insertion outro
Visit us at https://nursing.com/medical-disclaimer/ for disclaimer information.
NCLEX®, NCLEX-RN® are registered trademarks of the National Council of State Boards of Nursing, INC. and hold no affiliation with NURSING.com.