Top videos

The major elements of the cardiac exam include observation, palpation and, most importantly, auscultation (percussion is omitted). As with all other areas of the physical exam, establishing adequate exposure and a quiet environment are critical. Initially, the patient should rest supine with the upper body elevated 30 to 45 degrees. Most exam tables have an adjustable top. If not, use 2 or 3 pillows. Remember that although assessment of pulse and blood pressure are discussed in the vital signs section they are actually important elements of the cardiac exam.
Cluster headaches, which occur in cyclical patterns or clusters, are one of the most painful types of headache. A cluster headache commonly awakens you in the middle of the night with intense pain in or around one eye on one side of your head. Bouts of frequent attacks, known as cluster periods, can last from weeks to months, usually followed by remission periods when the headaches stop. During remission, no headaches occur for months and sometimes even years. Fortunately, cluster headache is rare and not life-threatening. Treatments can make cluster headache attacks shorter and less severe. In addition, medications can reduce the number of cluster headaches.

https://bit.ly/3HIStRc #shorts
Tracheotomy and tracheostomy are surgical procedures that create an opening in the trachea (windpipe) to help patients breathe when they have difficulty doing so through the nose or mouth. Though they are similar in purpose, there are some key differences between them.
Tracheotomy is a temporary procedure that involves creating a small incision in the trachea to insert a breathing tube. The tube is typically removed once the patient no longer requires it, and the incision heals on its own. Tracheostomy, on the other hand, is a more permanent solution that involves creating a hole in the trachea and inserting a tracheostomy tube, which remains in place for an extended period.
Indications for these procedures include:
Airway obstruction due to trauma, tumors, or infection
Severe respiratory distress or failure
Prolonged mechanical ventilation
Inability to protect the airway due to neurological disorders or impaired consciousness
Steps for performing a tracheotomy and tracheostomy:
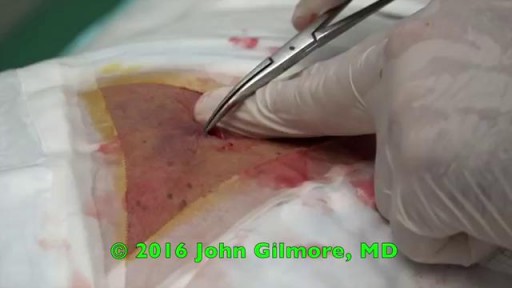
Preparation: The patient is positioned, and the neck area is cleaned and draped. Local anesthesia is often administered, although general anesthesia may be used in some cases.
Incision: A small incision is made in the neck, and the muscles and tissues are carefully separated to expose the trachea.
Tracheal opening: A small opening is made in the trachea, typically between the second and third tracheal rings.
Tube insertion: A tracheotomy tube is inserted through the incision and into the trachea for a tracheotomy, while a tracheostomy tube is inserted for a tracheostomy. Both tubes are secured in place.
Confirmation: Proper placement of the tube is confirmed by listening for breath sounds and checking for adequate ventilation.
Pre-operative care typically involves a thorough assessment of the patient's medical history, as well as any necessary imaging studies or lab tests to ensure the procedure is appropriate and safe. Informed consent should be obtained from the patient or their legal representative.
Post-operative care includes monitoring the patient's vital signs, ensuring the tube remains secure and patent, and managing any pain or discomfort. For tracheostomy patients, regular cleaning and maintenance of the stoma (the opening in the trachea) and the tracheostomy tube are essential to prevent infection and other complications. Long-term care may involve speech therapy, respiratory therapy, and support from a multidisciplinary team to address any ongoing needs.
It's crucial to remember that these procedures should only be performed by trained medical professionals in a clinical setting.
for additional information about this procedure check our article @ www.medicalartsshop.com
For more free resources, find us on Pinterest & Facebook pages:
https://www.pinterest.ca/medicalartsofficial/
https://www.facebook.com/Medicalartsofficial
https://www.youtube.com/@medic....alarts?sub_confirmat
https://www.instagram.com/medicalartsofficial/
https://www.tiktok.com/@medicalarts
This video and associated content are for entertainment and educational purposes only!!

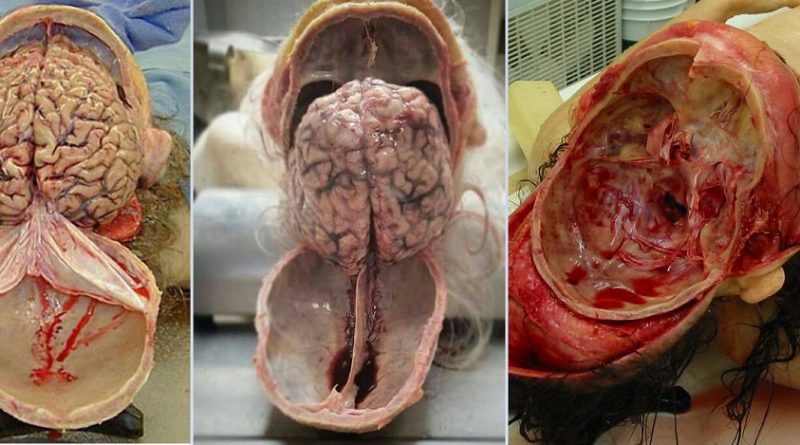
Doctors save the life of an unborn baby who was injured along with her mother in a missile attack in the Syrian city of Aleppo. The video shows a team of emergency medical workers delivering the baby by Cesarean section and then treating the newborn for the shrapnel wounds covering her body and one very large gash in her head. “Medics can be seen frantically reviving the baby, after delivering her by emergency cesarean, as she lies motionless,” the article states. “Eventually the tiny newborn begins to cry and seemingly comes to life as she is given an oxygen mask and rubbed vigorously.” “According to Reuters, the woman also has three other children, all of whom were injured in the attack, but are reported by doctors in the hospital to be in a good condition,” the Daily Mirror article states. The article does not provide the gestational age of the baby before it was delivered. The article said the pregnant woman was hit by a barrel bomb – “crude explosives and shrapnel and dropped from helicopters used by [Syrian] President Bashir al-Assad’s regime." The article notes an estimated 7.6 million Syrians have been displaced by the ongoing civil war and that 320,000, including 11,000 children, have been killed in the conflict. The Daily Mirror also reports that the doctors suggested that the tiny girl be named Amal, which means hope in Arabic. UK Daily Mirror: Incredible footage shows Syrian doctors perform lifesaving caesarean after missile strike leaves shrapnel embedded in unborn baby's face

This anatomical implant was originally placed in 1997. Due to the dark yellow color inside the implant it is clear the implant has been ruptured for quite some time. When implants rupture, it is important to have them replaced as soon as possible to avoid excessive scarring in the breasts. If too much scar tissue has accumulated around the deflated implant, it becomes difficult to create a normal breast shape in the future. Therefor its important to know the signs of a ruptured implant such as, painful to touch, visible asymmetry or loss of integrity to the bag. Dr. Stuart Linder 9675 Brighton Way Suite 420 Beverly Hills, CA 90210
Intestino Irritable Tratamiento, Colon Irritable, Tratamiento Para El Colon Irritable--- http://intestino-irritable-tratamiento.plus101.com --- Si usted está sufriendo de Síndrome del Intestino Irritable SII, aquí hay una serie de técnicas y estrategias que se conocen para aliviar grandemente los síntomas a largo y corto plazo. La alimentación es la fuente de energía primordial que tenemos y es por eso que hay que darle una importancia suprema a la hora de querer atacar los síntomas del SII. Se recomienda el consumo de hierbas, tales como: manzanilla, consuelda, aceite de onagra, bálsamo de limón, hinojo, canela, nuez moscada, cúrcuma, todas las especias y enzimas digestivas. Todas ellas producen grandes beneficios para su organismo, dentro de los cuales destacamos: La manzanilla actúa como carminativo, así como calmante y agente tonificante para el tracto digestivo. Los aceites esenciales de manzanilla también han contribuido a aliviar cólicos intestinales e irritación en los animales. La manzanilla se toma normalmente tres veces al día, entre las comidas, en una forma de té. La consuelda tiene un uso como agente tópico para mejorar la cicatrización de heridas, úlceras en la piel, tromboflebitis y torceduras. También se utiliza para las personas con problemas gastrointestinales, como úlceras de estómago y el síndrome del intestino irritable, y para quienes sufren problemas pulmonares. Una combinación de menta, comino y otras dos hierbas carminativas (para aliviar los gases), semillas de hinojo y ajenjo, han resultado ser un tratamiento eficaz para los dolores abdominales. La acacia tiene un alto contenido de fibra y con frecuencia se recomienda para aliviar la irritabilidad intestinal. Las frutas como la papaya, el plátano, el mango, la piña, las fresas y los arándanos son altamente recomendables. Las verduras como las patatas dulces, la calabaza y las zanahorias no pueden dejar de ser parte de su dieta. Tenga cuidado con algunos de los medicamentos recetados para el SII ya que algunos de ellos han sido retirados del mercado debido a que contenían ingredientes tóxicos. Algunos ingredientes contenidos en medicamentos de venta libre para el resfriado también han demostrado efectos negativos en pacientes con SCI. Recomendamos las gotas de zinc como una alternativa durante un resfriado ya que no irrita el estómago y tiene visibles resultados de estímulo inmunológico. Los alimentos que se deben evitar: lácteos, huevos (especialmente la yema debido al alto contenido de grasa), brócoli, maíz, aceites hidrogenados, jarabe de maíz alto en fructosa, manzanas (debido al alto contenido de fructosa), frijoles, chocolate (debido a la cafeína) , café, té con cafeína. Para obtener más información sobre cómo poder controlar y eliminar los síntomas del SII, puede visitar el sitio http://intestino-irritable-tratamiento.plus101.com

Traditionally, the appendix is removed through an incision in the right lower abdominal wall. In most laparoscopic appendectomies, surgeons operate through 3 small incisions (each ¼ to ½ inch) while watching an enlarged image of the patient's internal organs on a television monitor.