Top videos
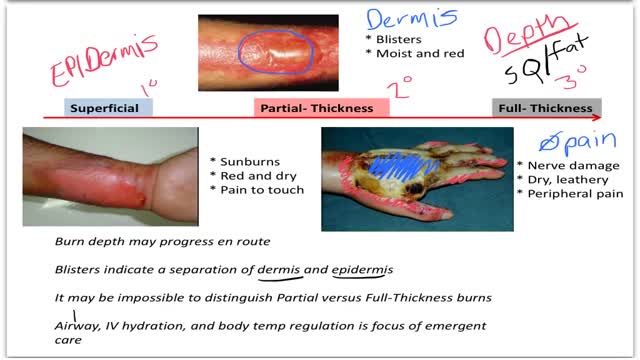
Burns are classified as first-, second-, or third-degree, depending on how deep and severe they penetrate the skin's surface. First-degree burns affect only the epidermis, or outer layer of skin. The burn site is red, painful, dry, and with no blisters. Mild sunburn is an example.

The cause for TS is unknown. Early research suggested that TS is an inherited condition (often, the person's near or distant relatives have had some form of transient or chronic tic disorder or associated symptoms). Recent studies point to a combination of environmental and genetic factors as a cause of the disorder. The specific genes involved in the development of TS are still being investigated. Studies suggest that TS has a neurological basis and results from an abnormality which affects the brain's metabolism of certain neurotransmitters (chemicals in the brain that regulate behavior.) Current research being funded by the Tourette Syndrome Association (TSA) will help provide more information about the causes and genetic factors of TS.

Marfan syndrome is a genetic disorder that affects the body's connective tissue. Connective tissue holds all the body's cells, organs and tissue together. It also plays an important role in helping the body grow and develop properly. Connective tissue is made up of proteins.

Dr. Ailawadi, M.D., the Chair of Cardiac Surgery at Michigan Medicine, specializes in minimally invasive valve surgery as well as complex cardiac operations. This video shows step by step footage of a Coronary Artery Bypass Graft (CABG) in a complex patient. In this case, CABG was performed through a sternotomy (through the breast bone) using the internal thoracic artery and saphenous leg veins to bypass obstructed coronary arteries. In this video, Dr. Ailawadi will perform a triple vessel bypass (CABG) which has been shown to minimize the risk of future heart attack and help patients live longer in the setting of complex coronary artery disease.
To learn more about cardiac surgery at Michigan Medicine, visit: https://medicine.umich.edu/dept/cardiac-surgery
To learn more about Frankel Cardiovascular Center, visit: https://www.umcvc.org/
To watch the full playlist, visit: https://www.youtube.com/playli....st?list=PLNxqP-XbH8B
-------------------------------------------------------
Subscribe to Michigan Medicine’s YouTube channel for upcoming videos and future live streams featuring our experts answering your questions.
-------------------------------------------------------
Follow Michigan Medicine on Social:
Twitter: https://twitter.com/umichmedicine
Instagram: https://www.instagram.com/umichmedicine/
Facebook: https://www.facebook.com/MichiganMedicine/
Follow the U-M Frankel Cardiovascular Center on Social:
Twitter: https://twitter.com/umichcvc
Facebook: https://www.facebook.com/Unive....rsityofMichiganCardi
#MichiganMedicine #MedEd #CardiacSurgery #UniversityOfMichiganHealth #FrankelCardiovascularCenter #Cardiology #CardiacSurgeon

Welcome to the latest episode of HT Physio Quick Tips!
In this episode, Farnham's leading over-50's physiotherapist, Will Harlow, reveals the most common knee injuries that can be sustained from a fall. You'll learn the 5 most common knee injuries from falls, how to differentiate between them and the key signs to look for before getting help.
To register your interest for the upcoming Optimum Knee Health course and to be among the first to know when it is released, reach out to Will@ht-physio.co.uk
To get a copy of Will's new book, Thriving Beyond Fifty, you can find it on Amazon below:
UK link: https://amzn.to/3mAISFv
US link: https://amzn.to/43TE5Q8
(Amazon Affiliate links)
If you're suffering from nagging knee pain that hurts in the morning and stops you from walking as far as you'd like, you can take our free knee pain guide - which will give you 5 expert tips to put a stop to knee pain at home - by visiting here: https://ht-physio.co.uk/knee-pain-guide-download/
If you're over-50 with a painful problem in the Farnham, Surrey area, you can learn more about how Will Harlow and HT Physio can help you overcome a painful problem here: https://ht-physio.co.uk/
**Any information in this video should not be used as a substitute for individual medical advice. Please seek advice from your local healthcare professional before taking action on the information in this video.**

Intrauterine insemination (IUI) is a fertility treatment that involves placing sperm inside a woman's uterus to facilitate fertilization. The goal of IUI is to increase the number of sperm that reach the fallopian tubes and subsequently increase the chance of fertilization
Bartter syndrome is a rare inherited defect in the thick ascending limb of the loop of Henle. It is characterized by low potassium levels (hypokalemia), increased blood pH (alkalosis), and normal to low blood pressure. There are two types of Bartter syndrome: neonatal and classic

You can now test your knowledge with a free lesson quiz on NURSING.com!
Click here for your free quiz: https://bit.ly/3GF9I3h
NG (Nasogastric) Tube Insertion Techniques (Nursing Skills)
FREE Nursing School Cheat Sheets at: http://www.NURSING.com
Get the full lesson on NG Tube Insertion here:
https://nursing.com/lesson/ski....lls-04-01-inserting-
Get Access to Thousands of Lessons here:
https://nursing.com/courses/
Welcome to the NURSING Family, we call it the most supportive nursing cohort on the planet.
At NURSING.com, we want to help you remove the stress and overwhelm of nursing school so that you can focus on becoming an amazing nurse.
Check out our freebies and learn more at: (http://www.nursing.com)
NG (Nasogastric) Tube Insertion Techniques (Nursing Skills)
In this video we’re going to show you the correct technique for insertion of an NG tube or Nasogastric tube). We’ll also give you a few tips and tricks we use. Of course, before you get started, make sure you’ve determined which nare is more patent and that the patient doesn’t have a deviated septum. Before you start, lay a towel across the patient’s chest – I’m telling you I’ve had patients throw up on me – this step is WORTH IT!! We love you guys! Go out and be your best selves today! And, as always, happy nursing!
Bookmarks:
0.05 Introduction to NG Tube Insertion techniques
0.25 Towel placement
0.32 Measuring NG tube length
1.04 Tape preparation
1.27 Give patient water
1.34 NG Tube lubrication
1.42 NG Tube insertion technique
2.25 Securing the NG tube
2.36 Checking placement/ aspiration
2.55 Assessing pH
3.08 Confirming placement
3.22 Waiting for abdominal X-ray
3.35 Supply clean-up
3.48 NG Tube insertion outro
Visit us at https://nursing.com/medical-disclaimer/ for disclaimer information.
NCLEX®, NCLEX-RN® are registered trademarks of the National Council of State Boards of Nursing, INC. and hold no affiliation with NURSING.com.

How to perform a Thyroid Gland Examination - Clinical Skills Revision
The thyroid examination is one of the first sessions of the clinical skills block for medical students at Warwick Medical School - largely as it touches lightly on to other clinical areas, such as the cardiac examination, and the peripheral neurological examination making it an excellent starting point for building further knowledge
This is a clinical examination of the thyroid gland is performed by Dr James Gill following the approach in Macleod’s Clinical examination.
------------------
Please note that there is no ABSOLUTE way to perform a clinical examination. Different institutions and even clinicians will have differing degrees of variations - the aim is the effectively identify medically relevant signs.
However, during OSCE assessments. Different medical schools, nursing colleges and other health professional courses will have their own preferred approach to a clinical evaluation - you should concentrate on THEIR marks schemes for your assessments.
The examination demonstrated here is derived from Macleods Clinical Examination - a recognised standard textbook for clinical skills.
Some people may experience an ASMR effect from watching this medical clinical examination
#ThyroidExamination #ClinicalSkills #DrGill #ASMR

Detroit TV meteorologist Jessica Starr posted a heart-wrenching video on social media a month before dying by suicide this week. She had told viewers she was struggling in the aftermath of undergoing Lasik surgery. After learning of her death, her heartbroken colleagues on WJBK fought back tears live on TV. Twelve people have died by suicide after suffering pain and even blindness after the operation. Inside Edition also spoke to a doctor who wants the surgery banned. #InsideEdition