Top videos
The most common position of the uterus is anteverted (cervix angles forward) and anteflexed (body is flexed forward). The position of the uterus in the adult is liable to considerable variation, depending chiefly on the condition of the bladder and rectum. Adnexa: In gynecology, the appendages of the uterus, namely the ovaries, the Fallopian tubes, and the ligaments that hold the uterus in place.
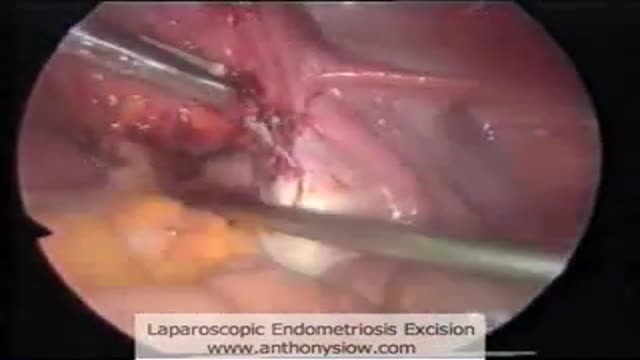
Laparoscopic excision of endometriosis
Ophthalmoscopic exam
Mitral valve repair of anterior leaflet perforation and ruptured chordae
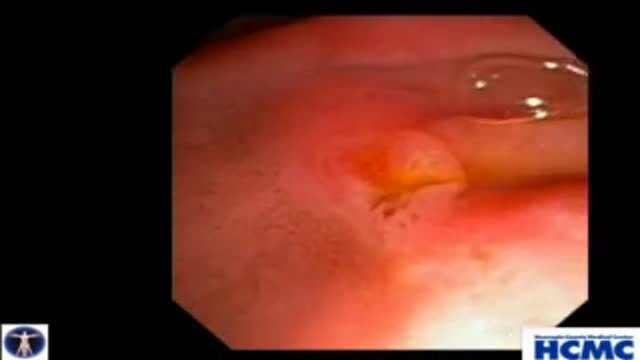
Small colon polyp (redish bump)and many diverticuli (small outpouches in wall of the colon)
Examination of the cervical spines
• Define and use related medical terminology.
• Describe and demonstrate techniques for imaging the thyroid gland.
• Discuss functional abnormalities of the thyroid gland.
• Correlate laboratory data relevant to the thyroid and parathyroid glands.
• Describe, and recognize on images, pathologies of the thyroid gland.
• Identify the anatomy of the parathyroid glands on diagrams and sonograms.
• Describe and demonstrate techniques for imaging the parathyroid glands.
• Describe, and recognize on images, pathologies of the parathyroid glands.
• List and describe other neck masses.
• Follow relevant protocols when scanning.
• Differentiate the sonographic appearances of the female reproductive organs in relation to the menstrual cycle, the use of contraceptives and hormone replacement, and following chemotherapy.
• Explain the Patient Privacy Rule (HIPAA) and Patient Safety Act (see reference).
Watch that video of Unbelievable Mutations and Medical Conditions
Hawkin's Test
indicated in Radius and Ulna Fractures
Sensory and reflexes exam of the upper limb from the USMLE collection Sensory and reflexes exam of the upper limb
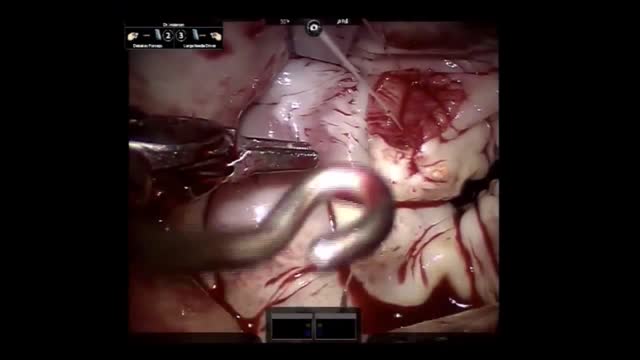
Total Laparoscopic Hysterectomy
Bronchiectasis is an abnormal dilation of the proximal and medium-sized bronchi (>2 mm in diameter) caused by weakening or destruction of the muscular and elastic components of the bronchial walls. Affected areas may show a variety of changes, including transmural inflammation, edema, scarring, and ulceration, among other findings. Distal lung parenchyma may also be damaged secondary to persistent microbial infection and frequent postobstructive pneumonia. Bronchiectasis can be congenital but is most often acquired.[9] Congenital bronchiectasis usually affects infants and children. These cases result from developmental arrest of the bronchial tree. Acquired forms occur in adults and older children and require an infectious insult, impairment of drainage, airway obstruction, and/or a defect in host defense. The tissue is also damaged in part by the host response of neutrophilic proteases, inflammatory cytokines, nitric oxide, and oxygen radicals. This results in damage to the muscular and elastic components of the bronchial wall. Additionally, peribronchial alveolar tissue may be damaged, resulting in diffuse peribronchial fibrosis.[12] The result is abnormal bronchial dilatation with bronchial wall destruction and transmural inflammation. The most important functional finding of altered airway anatomy is severely impaired clearance of secretions from the bronchial tree. Impaired clearance of secretions causes colonization and infection with pathogenic organisms, contributing to the purulent expectoration commonly observed in patients with bronchiectasis. The result is further bronchial damage and a vicious cycle of bronchial damage, bronchial dilation, impaired clearance of secretions, recurrent infection, and more bronchial damage
Continuous Lumbar Epidural
Watch that Real Human Body Decomposing Process On Video
Sclerotherapy for varicose veins
This 38 year old woman has increasingly intractable RUQ pain after cholecystectomy done one year prior. LFTs and pancreatic enzymes have been normal, and ducts are non-dilated, thus she is a Type III possible SOD patient. Initial goal is to define course of pancreatic duct for manometry. 5-4-3 Co...ntour catheter (Boston Scientific) is used to perform the pancreatogram which shows a small straight distal duct. The aspirating triple lumen manometry catheter (Wilson Cook) is used to cannulate the pancreatic duct, with continuous aspiration of fluid once the duct is entered. Careful stationed pullthrough manometry shows markedly abnormal basal pressures in both leads in the pancreatic sphincter. Plan is dual pancreatic and biliary sphincterotomy. Biliary manometry will not now change our plan therefore is omitted. Our first goal is to access the pancreatic duct so we can guarantee wire access for placement of a small caliber pancreatic stent which is critical for safety. Contrast is injected as the 0.018in Roadrunner wire (Wilson Cook) is advanced in order to outline the course of main duct. A separate biliary orifice is clearly seen, unusual in SOD patients. A soft 4Fr 3cm single inner flange pancreatic stent (Hobbs Medical) is placed. We did not want to use our typical 9cm long unflanged stent as even a 3 or 4 French stent might be traumatic to the tiny caliber of this duct out in the body of the gland. Next the bile duct is cannulated with a papillotome (Autotome 39, Boston Scientific), showing a small perhaps 6mm bile duct. Biliary sphincterotomy is performed in very careful stepwise fashion as landmarks are unclear and perforation is higher risk in small duct SOD patients. On the other hand, inadequate sphincterotomies offer limited chance of symptom relief. You can see here a patulous sphincterotomy. Next a pancreatic sphincterotomy is performed with the needle knife (Boston Scientific) over the pancreatic stent. Again this is performed cautiously due to the small size of the pancreatic duct. We are reaching along the stent and cutting the fibers deeply. This is a limited pancreatic sphincterotomy due to small pancreatic duct size, and concern for scarring of the pancreatic duct. It is important to document passage of the stent by xray or remove it endoscopically with two weeks or so. We and many other specialized centers perform dual sphincterotomies at the first ERCP in all SOD patients with abnormal pancreatic manometry and frequent or intractable symptoms based on the belief that response rates are better than for biliary sphincterotomy alone.
A simple video showing the small tips to be followed by patients which a clinician should provide. The video is simple, easy to understand and can be provided to the patient for their reference.
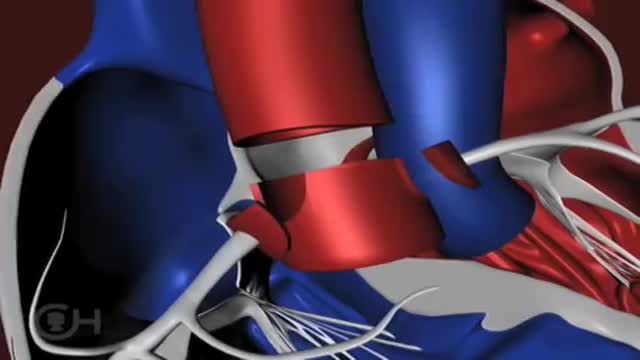
The "great arteries" in this anomaly refer to the aorta and the pulmonary artery, the two major arteries carrying blood away from the heart. In cases of transposition of the great arteries, these vessels arise from the wrong ventricle. They are "transposed" from their normal position so that the aorta arises from the right ventricle and the pulmonary artery from the left ventricle. Other heart defects may occur along with transposition of the great arteries. About 25 percent of children with transposition will also have a ventricular septal defect (VSD) . In nearly a third, the branching pattern of the coronary arteries as they leave the transposed aorta is unusual. Infants may also have narrowing below the pulmonary valve that blocks blood flow from the left ventricle to the lungs.