Top videos

A 28 years old man lost his right arm with a conveyor device in 2014. The video is taken 2 years after replantation. You can see another videos in my site: https://drliaghatclinic.com, https://instagram.com/liaghatclinic, https://t.me/liaghatclinic

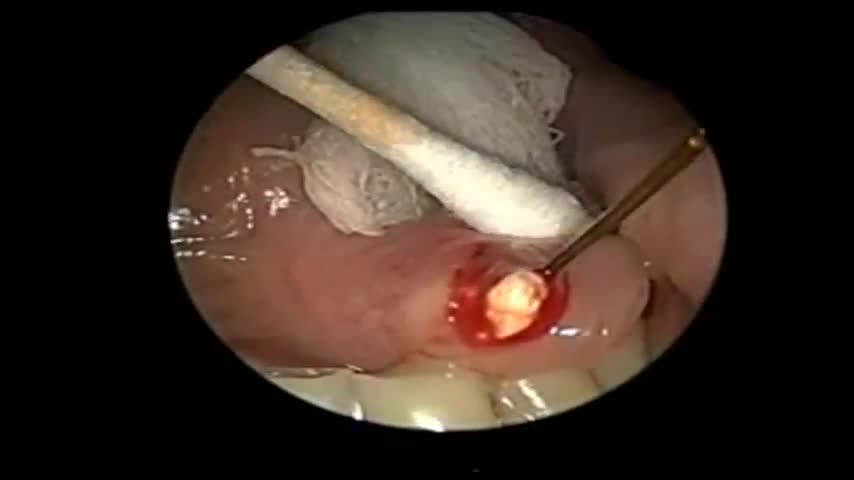
How to perform a parotidectomy gland resection? In this video we take you step by step through the protid gland resection surgical technique. This video is intended for ENT residents and Head and Neck Surgery Surgeons. It is part of the ORL-Information's Head and Neck surgery Masterclass in collaboration with the University Hospital of Nîmes. Surgeons Editors: Pr. Benjamin LALLEMANT, MD, PhD - Dr. Camille GALY, MD Head and and Neck Department, University Hospital of Nîmes, France Official video | www.orl-information.fr
Cette vidéo présentent la technique de la parotidectomie avec dissection du nerf facial. Elle illustre les différents temps de l'intervention notamment le temps de repérage du nerf facial.
--------------------------------------
@Prévention médecine | Comment préserver sa santé ?
✔Abonnez-vous à la chaîne ORL-Information : https://www.youtube.com/c/ORLINFORMATION
✔Retrouvez-nous sur internet: https://www.orl-information.fr

Orthopedic spine surgeons and vascular surgeons at UW Health in Madison, WI work together to perform minimally invasive anterior lumbar interbody fusion (Mini-ALIF). With this type of spinal fusion surgery, patients have smaller incisions, usually spend less time in the hospital and typically return to daily activities more quickly. Learn more https://www.uwhealth.org/ALIF
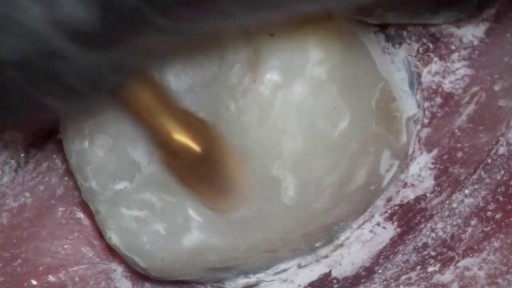
Sialendoscopy can be both diagnostic and therapeutic. It is complementary to diagnostic techniques such as plain radiography, ultrasonography, computed tomography (CT), magnetic resonance sialography, and conventional sialography, all of which are traditional, time-tested methods for evaluating the salivary ductal system

The pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region (including perineum) below.
The right and left levator ani lie almost horizontally in the floor of the pelvis, separated by a narrow gap that transmits the urethra, vagina, and anal canal. The levator ani is usually considered in three parts: pubococcygeus, puborectalis, and iliococcygeus. The pubococcygeus, the main part of the levator, runs backward from the body of the pubis toward the coccyx and may be damaged during parturition. Some fibers are inserted into the prostate, urethra, and vagina. The right and left puborectalis unite behind the anorectal junction to form a muscular sling . Some regard them as a part of the sphincter ani externus. The iliococcygeus, the most posterior part of the levator ani, is often poorly developed.
The coccygeus, situated behind the levator ani and frequently tendinous as much as muscular, extends from the ischial spine to the lateral margin of the sacrum and coccyx.
The pelvic cavity of the true pelvis has the pelvic floor as its inferior border (and the pelvic brim as its superior border.) The perineum has the pelvic floor as its superior border.
Some sources do not consider “pelvic floor” and “pelvic diaphragm” to be identical, with the “diaphragm” consisting of only the levator ani and coccygeus, while the “floor” also includes the perineal membrane and deep perineal pouch.

Ganglion cysts are noncancerous lumps that most commonly develop along the tendons or joints of your wrists or hands. They also may occur in the ankles and feet. Ganglion cysts are typically round or oval and are filled with a jellylike fluid. Small ganglion cysts can be pea-sized, while larger ones can be around an inch (2.5 centimeters) in diameter. Ganglion cysts can be painful if they press on a nearby nerve. Their location can sometimes interfere with joint movement. If your ganglion cyst is causing you problems, your doctor may suggest trying to drain the cyst with a needle. Removing the cyst surgically also is an option. But if you have no symptoms, no treatment is necessary. In many cases, the cysts go away on their own.

Elizabeth Stephens, MD joined the Department of Cardiovascular Surgery at Mayo Clinic Rochester, Minnesota in 2019. To learn more about Dr. Stephens’ practice: https://www.mayoclinic.org/bio....graphies/stephens-el
Elizabeth H. Stephens, M.D., Ph.D., is an Assistant Professor of Surgery in Cardiovascular Surgery specializing in congenital cardiac surgery. She received her medical degree from Baylor College of Medicine and Ph.D in Bioengineering from Rice University focusing on tissue engineering heart valves. Her adult cardiothoracic training was completed at Columbia University and congenital training at Lurie Children's Hospital in Chicago. Her clinical areas of expertise include the treatment of:
• Neonates, infants, and children with complex congenital heart disease
• Adult patients with congenital heart disease, including patients previously repaired
• Valve disease, including Ebstein's anomaly
• Pediatric patients with heart failure, including mechanical circulatory support and heart transplantation
• Patients with vascular rings and tracheal stenosis
In addition to her clinical areas of expertise, Dr. Stephens is active in outcomes research relative to congenital heart disease and is extensively published on various cardiac surgery conditions. She has a particular interest in education, including serving on national committees and mentoring trainees of all levels.
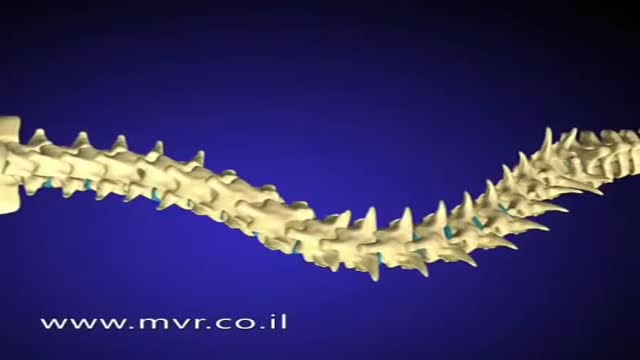
There are several approaches to scoliosis surgery, but all use modern instrumentation systems in which hooks and screws are applied to the spine to anchor long rods. The rods are then used to reduce and hold the spine while bone that is added fuses together with existing bone.