Top videos
Vitiligine News, Vitiligine Foto, Vitiligine Come Si Manifesta, La Vitiligine, Rimedi Vitiligine --- http://vitiligine-cura.good-info.co --- Non Importa Quanto Sia Grave La Tua Vitiligine, Puoi Iniziare A Utilizzare Questo Sistema Potente PROPRIO ORA Per Ottenere La Libertà Dalla Vitiligine Che Hai Sempre Sognato! Funziona In Tutti I Casi Seguenti: Vitiligine Leggera, Moderata O Grave Vitiligine Focale Vitiligine Segmentale Vitiligine Mucoidale Vitiligine acrofacciale Vitiligine vulgaris Vitiligine universale I trattamenti anti-vitiligine che la maggior parte della gente usa NON FUNZIONANO! Il 95% di tutti quelli che trattano la vitiligine finisce peggio di quando ha iniziato! Una Presentazione Video Gratuita Spiega Un Singolare Consiglio Per Eliminare La Vitiligine Per Sempre http://vitiligine-cura.good-info.co

The pelvic diaphragm is composed of muscle fibers of the levator ani, the coccygeus, and associated connective tissue which span the area underneath the pelvis. The pelvic diaphragm is a muscular partition formed by the levatores ani and coccygei, with which may be included the parietal pelvic fascia on their upper and lower aspects. The pelvic floor separates the pelvic cavity above from the perineal region (including perineum) below.
The right and left levator ani lie almost horizontally in the floor of the pelvis, separated by a narrow gap that transmits the urethra, vagina, and anal canal. The levator ani is usually considered in three parts: pubococcygeus, puborectalis, and iliococcygeus. The pubococcygeus, the main part of the levator, runs backward from the body of the pubis toward the coccyx and may be damaged during parturition. Some fibers are inserted into the prostate, urethra, and vagina. The right and left puborectalis unite behind the anorectal junction to form a muscular sling . Some regard them as a part of the sphincter ani externus. The iliococcygeus, the most posterior part of the levator ani, is often poorly developed.
The coccygeus, situated behind the levator ani and frequently tendinous as much as muscular, extends from the ischial spine to the lateral margin of the sacrum and coccyx.
The pelvic cavity of the true pelvis has the pelvic floor as its inferior border (and the pelvic brim as its superior border.) The perineum has the pelvic floor as its superior border.
Some sources do not consider “pelvic floor” and “pelvic diaphragm” to be identical, with the “diaphragm” consisting of only the levator ani and coccygeus, while the “floor” also includes the perineal membrane and deep perineal pouch.

Check out our new website http://www.evanshealthlab.com/
Follow Dr. Mike for new videos! http://twitter.com/docmikeevans
Dr. Mike Evans is founder of the Health Design Lab at the Li Ka Shing Knowledge Institute, an Associate Professor of Family Medicine and Public Health at the University of Toronto, and a staff physician at St. Michael's Hospital.
Written and Narrated by Dr. Mike Evans
Executive Producer, Dr. Mike Evans
Illustrations by Liisa Sorsa
Produced, Directed, and Photographed by Nick De Pencier
Editor, David Schmidt
Story/Graphic Facilitator, Disa Kauk
Production Assistant, Chris Niesing
Director of Operations, Mike Heinrich
©2014 Michael Evans and Reframe Health Films Inc.
Intestino Irritable Tratamiento, Colon Irritable, Tratamiento Para El Colon Irritable--- http://intestino-irritable-tratamiento.plus101.com --- Si usted está sufriendo de Síndrome del Intestino Irritable SII, aquí hay una serie de técnicas y estrategias que se conocen para aliviar grandemente los síntomas a largo y corto plazo. La alimentación es la fuente de energía primordial que tenemos y es por eso que hay que darle una importancia suprema a la hora de querer atacar los síntomas del SII. Se recomienda el consumo de hierbas, tales como: manzanilla, consuelda, aceite de onagra, bálsamo de limón, hinojo, canela, nuez moscada, cúrcuma, todas las especias y enzimas digestivas. Todas ellas producen grandes beneficios para su organismo, dentro de los cuales destacamos: La manzanilla actúa como carminativo, así como calmante y agente tonificante para el tracto digestivo. Los aceites esenciales de manzanilla también han contribuido a aliviar cólicos intestinales e irritación en los animales. La manzanilla se toma normalmente tres veces al día, entre las comidas, en una forma de té. La consuelda tiene un uso como agente tópico para mejorar la cicatrización de heridas, úlceras en la piel, tromboflebitis y torceduras. También se utiliza para las personas con problemas gastrointestinales, como úlceras de estómago y el síndrome del intestino irritable, y para quienes sufren problemas pulmonares. Una combinación de menta, comino y otras dos hierbas carminativas (para aliviar los gases), semillas de hinojo y ajenjo, han resultado ser un tratamiento eficaz para los dolores abdominales. La acacia tiene un alto contenido de fibra y con frecuencia se recomienda para aliviar la irritabilidad intestinal. Las frutas como la papaya, el plátano, el mango, la piña, las fresas y los arándanos son altamente recomendables. Las verduras como las patatas dulces, la calabaza y las zanahorias no pueden dejar de ser parte de su dieta. Tenga cuidado con algunos de los medicamentos recetados para el SII ya que algunos de ellos han sido retirados del mercado debido a que contenían ingredientes tóxicos. Algunos ingredientes contenidos en medicamentos de venta libre para el resfriado también han demostrado efectos negativos en pacientes con SCI. Recomendamos las gotas de zinc como una alternativa durante un resfriado ya que no irrita el estómago y tiene visibles resultados de estímulo inmunológico. Los alimentos que se deben evitar: lácteos, huevos (especialmente la yema debido al alto contenido de grasa), brócoli, maíz, aceites hidrogenados, jarabe de maíz alto en fructosa, manzanas (debido al alto contenido de fructosa), frijoles, chocolate (debido a la cafeína) , café, té con cafeína. Para obtener más información sobre cómo poder controlar y eliminar los síntomas del SII, puede visitar el sitio http://intestino-irritable-tratamiento.plus101.com
Ejaculating into a partner’s mouth is a common practice during oral sex/fellatio. In a safe situation (where there is no danger of catching an STD), the semen-receiving partner may choose to spit the semen out, or to swallow it. Before you engage in fellatio, I’d recommend that you and your partner both get tested for sexually transmitted infections (STIs). If not, please use barriers for oral sex and abstaining from making contact with ejaculate. Semen is mostly water, but also contains amino acids and protein, sugars such as fructose and glucose, minerals such as zinc and calcium, vitamin C, and a few other nutrients. Sperm cells themselves make up less than one percent of semen. Semen is edible, and if swallowed, will travel down the esophagus and into the stomach, where it will be digested in the same way that food is. You can never get pregnant by swallowing semen. Some people accept the taste of semen, but others complain that swallowing semen can give them an upset stomach. In rare cases, you may have an allergy to the proteins found in semen. What does It Taste Like? The taste of semen varies. Bitter, sweet, metallic. So, one may expect to find the taste of semen anywhere from enjoyable to tasteless to disgusting. But there is a way of controlling the taste of semen, which is through diet. Keep track of the diet, and communicate with the partner about when it tastes better or worse.

An excellent video demonstrating how a laparoscopy is performed to evaluate the uterus (note a small fibroid appearing as a bulge in the uterus), fallopian tubes and ovaries. Blue dye is injected into the uterus, entering the fallopian tubes and spilling from the end of the tubes into the abdominal cavity, confirming that both tubes are open
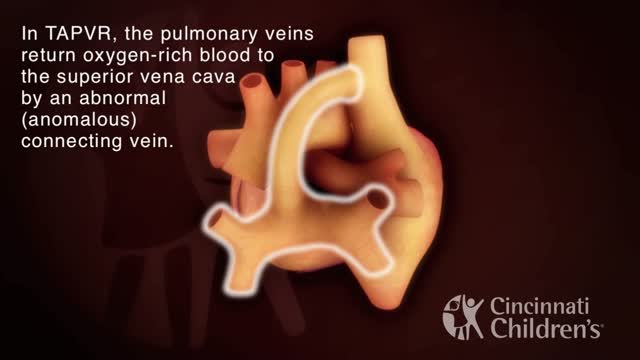
Total anomalous pulmonary venous return (TAPVR) is a rare congenital malformation in which pulmonary veins that return oxygen-rich blood from the lungs do not connect normally to the left atrium. Instead all four pulmonary veins drain abnormally to the right atrium. Heart models and animation were developed by the Cincinnati Children's Heart Institute in conjunction with Cincinnati Children's Critical Care Media Lab.

Liposuction is a surgical procedure that is done to remove fat deposits from underneath the skin. Common areas that are treated: the abdomen, buttocks, thighs, upper arms, chest and neck. (use medical graphic of body with labeled parts) The procedure is usually done as an outpatient under some combination of local anesthesia and/or sedation:. This means you are awake but relaxed and pain free. Depending on the number of areas to be treated and the specific technique selected, it may take from one to several hours. A small incision (cut) is made through the skin near the area of the fat deposit. Multiple incisions may be needed if a wide area or multiple areas are being done. A long hollow tube called a cannula will be inserted through this incision. Prior to inserting the cannula, the doctor may inject a solution of salt water that contains an anesthetic (numbing) medication and another medication to decrease bleeding. The cannula is then inserted and moved under the skin in a way to loosen the fat deposits so they may be suctioned out. Because a significant amount of body fluid is removed with the fat, an intravenous (through the veins) fluid line will be kept going during the procedure.
A recent technique called “ultrasound-assisted lipoplasty” uses a special cannula that liquefies the fat cells with ultrasonic energy. You should ask your doctor which technique he/she will use and how it will affect the type of anesthesia you will need and the length of the procedure.
Why is this procedure performed?
Liposuction is done to restore a more normal contour to the body. The procedure is sometimes described as body sculpting. It should be limited to fat deposits that are not responsive to diet and exercise. It is suggested that you should be within 20of your ideal body weight at the time of surgery. If you are planning to lose weight you should delay this procedure. This is not obesity surgery. The maximum amount of fat that can be removed is usually less than 10 pounds. The best results are achieved in people who still have firm and elastic skin. Although rare, there are risks and complications that can occur with liposuction. You should be aware that all the complications are increased if you are a smoker. You will need to quit smoking or at least avoid smoking for a month before and after surgery. If you have had prior surgeries near any of the areas to be treated, this may increase the risk of complications and you should discuss this with your doctor. Any history of heart disease, diabetes, bleeding problems or blood clots in your legs may make you more prone to post-operative problems and you should discuss these with your doctor. Finally, as with any cosmetic procedure it is important to have realistic expectations. The goals, limitations, and expectations of the procedure should be discussed openly and in detail with your doctor. Most insurance companies do not cover cosmetic surgery.
What should I expect during the post-operative period?
After surgery you should be able to go home but you will need someone to drive you. In the first few days after surgery it is common for the incisions to drain fluid and you will have to change dressings frequently. Fresh blood is not usual and if you have any bleeding you should call your doctor immediately. In some cases a small tube may have been placed through the skin to allow drainage. You will be limited to sponge baths until the drains and dressings are removed. After that you may take showers but no baths for 2 weeks. You may experience pain, burning, and numbness for a few days. Take pain medicine as prescribed by your doctor. You may notice a certain amount of bruising and swelling. The bruising will disappear gradually over 1 to 2 weeks. Some swelling may last for up to 6 months. If you have skin sutures they will be removed in 7 to 10 days. You should be able to be up and moving around the house the day after surgery but avoid any strenuous activity for about 1
What is hemodialysis and how does it work? Who needs it? How do you prepare for it? In the United States, over 30 million Americans have kidney disease, and sometimes, kidney disease progresses to kidney failure or end-stage renal disease. When this happens, you cannot survive unless you have a kidney transplant or some form of dialysis. So today we're going to talk about hemodialysis.
Your kidneys are the two kidney bean-shaped organs that are located in your lower back, or in your flanks. And the kidneys are responsible for filtering out or cleaning your blood. They get rid of excess waste, excess toxins, and excess fluids. If your kidneys stop functioning, then you develop renal failure or end-stage renal disease.
What is Hemodialysis?
Hemodialysis, or blood dialysis, is the filtering of your blood outside of your body. So, if your kidneys stop working properly, the hemodialysis acts as a substitute kidney. Now it's important to note that hemodialysis does not actually correct your own kidney function. It does not fix or treat your kidneys.
#hemodialysis #drfrita
What is The Dialyzer?
The dialyzer is actually the filter. It's the main powerhouse of the hemodialysis system, and it is what actually acts as the substitute kidney. In the dialyzer, you have these hollow fibers that run through it, and these fibers are bathed in something called dialysates, or dialysis fluid.
How Often Are Patients Treated With Hemodialysis?
Most patients who are on hemodialysis are on it between three and six hours, about three days a week, especially if they go to a center.
How Does Hemodialysis Work?
So when you are on dialysis, how does your blood get from your body to the hemodialysis machine and then back to your body? Well, it does so through tubes, and those tubes are connected to your access, and we'll talk about access in just a moment. But as far as the tubing, the tubing is connected to your body.
Types Of Hemodialysis Access
Arteriovenous Fistula or AV Fistula
The AV fistula is the gold standard as far as hemodialysis access is concerned because it gives you the most efficient hemodialysis and it is the least likely to be infected.
Arteriovenous Graft or AV Graft
The AV graft is very similar to the AV fistula in that you still have a surgically connected artery and a vein, usually in the arm, but in the case where if you have veins that are rather thin or arteries that are thin and maybe too weak in order to really give you a properly functioning, substantial AV fistula, then the vascular surgeon may opt to add an artificial material in order to make that shunt a little stronger, or little more durable. And so, an AV graft is another option for dialysis access.
Catheter
If you're in a situation where you need temporary dialysis, or if you have acute kidney injury, then you may have a temporary Vascath placed, and it's usually placed in a vein of the neck, the internal jugular vein, or it can be placed in the groin, or in the femoral vein.
Who Needs Hemodialysis Treatment?
How do you know if you need hemodialysis, and when is it time to prepare? Well, if you follow up with your kidney doctor (nephrologist) regularly, he or she will be watching your labs. They'll be able to see those signs of your kidneys not functioning properly.