Top videos

Check out our new website http://www.evanshealthlab.com/
Follow Dr. Mike for new videos! http://twitter.com/docmikeevans
Dr. Mike Evans is founder of the Health Design Lab at the Li Ka Shing Knowledge Institute, an Associate Professor of Family Medicine and Public Health at the University of Toronto, and a staff physician at St. Michael's Hospital.
Written and Narrated by Dr. Mike Evans
Executive Producer, Dr. Mike Evans
Illustrations by Liisa Sorsa
Produced, Directed, and Photographed by Nick De Pencier
Editor, David Schmidt
Story/Graphic Facilitator, Disa Kauk
Production Assistant, Chris Niesing
Director of Operations, Mike Heinrich
©2014 Michael Evans and Reframe Health Films Inc.
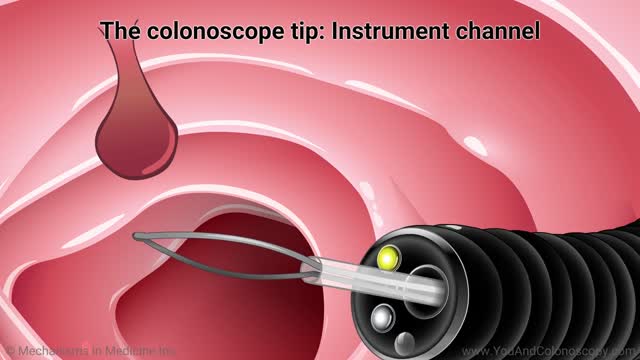
A colonoscope is the special tool used to perform a colonoscopy. It is a thin, flexible, tubular ‘telescope’ with a light and video camera that your doctor carefully guides through your colon in order to see and determine the health of your colon. Watch this animation to learn about the features of the colonoscope, how the colonoscopy procedure is performed and how polyps are removed, and the follow-up care you and your doctor should talk about after your procedure.
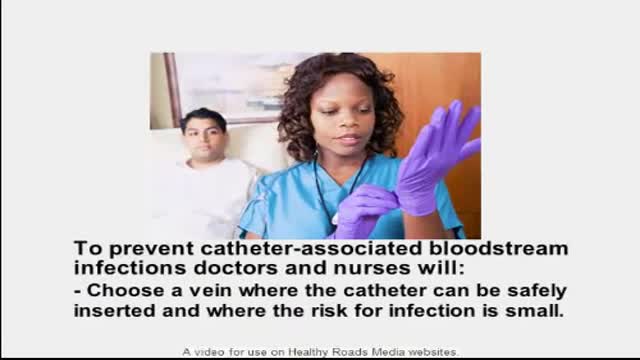
systemic inflammatory response syndrome (SIRS). This is most likely secondary to sepsis from an infection of the patient's Hickman catheter given the associated skin findings, although culture results are needed to confirm this diagnosis. The patient's low blood pressure is likely secondary to developing septic shock, and he has already appropriately been treated with intravenous fluids. Catheter removal is indicated given his hemodynamic instability. Catheter removal is also indicated in patients with severe sepsis with organ hypoperfusion, endocarditis, suppurative thrombophlebitis, or persistent bacteremia after 72 hours of appropriate antibiotic therapy. Long term catheters should also be removed if culture results are positive for S. aureus, P. aeruginosa, fungi, or mycobacteria.

Orthopedic spine surgeons and vascular surgeons at UW Health in Madison, WI work together to perform minimally invasive anterior lumbar interbody fusion (Mini-ALIF). With this type of spinal fusion surgery, patients have smaller incisions, usually spend less time in the hospital and typically return to daily activities more quickly. Learn more https://www.uwhealth.org/ALIF

Step in the Clinic with Dr. Pritesh Singh and get a practical insight into the Clinical Examination of Incisional Hernia.
Now Save Time with these Exam Relevant Clinical Videos & Waste None Studying Rare Cases.
Prepare with 2021 Dream Pack. It includes everything you need to ace Medical PG Entrance Exams. To enroll or know more visit: https://premium.prepladder.com/
=======================================================
To experience PrepLadder's excellent learning, download the app:
iOS: https://bit.ly/prepladderios
Android: https://bit.ly/prepladderandroid
Follow us on Social Media for all the latest updates:
Facebook: https://www.facebook.com/medic....al.pg.entrance.prepl
Instagram: https://www.instagram.com/prepladder_med
Subscribe to our YouTube channel and press the bell icon for more videos and regular updates: https://www.youtube.com/channe....l/UCdbMxSVAgPENqhYVe
#PrepLadder #ClinicalEssentials #PadhoWoChahiyeJo #DrPriteshSingh #Surgery #NEETPG #IncisionalHernia #2021DreamPack