Top videos

A seizure occurs when there’s abnormal electrical activity in the brain. Seizures may go virtually unnoticed. Or, in severe cases, they may produce a change or loss of consciousness and involuntary muscle spasms called convulsions. Seizures usually come on suddenly and vary in duration and severity. A seizure may be a one-time event, or you may have seizures repeatedly. Recurrent seizures are called epilepsy, or a seizure disorder. Less than one in 10 people who has a seizure develops epilepsy. Experts classify seizures into two general categories and many subtypes based on the pattern of the attack. Generalized seizures involve both sides of the brain from the start of the attack. Common subtypes include tonic-clonic (grand mal) and absence seizures (petit mal). Febrile and infantile spasms are two types of generalized seizures that occur almost exclusively in young children. Partial (or focal) seizures are the second major seizure type. These begin in a specific area of the brain and may be contained there. Or they may spread to the entire brain. With simple partial seizures, the person remains conscious. Complex partial seizures involve impaired consciousness. What Causes Seizures? Often the cause of a seizure is unknown. Many conditions can provoke seizures, including: Stroke Brain tumors Head injuries Electrolyte imbalance Very low blood sugar Repetitive sounds or flashing lights, such as in video games Medications, such as antipsychotics and some asthma drugs Withdrawal from medications, such as Xanax, narcotics, or alcohol Use of drugs such as cocaine and heroin Cancer Brain infections, such as meningitis

In this video, we show a sports hernia self treatment we give many of our clients. It is not the only part of treatment. Grabbing the skin around the region of the groin strain can reduce pain and stiffness with turning and twisting. Sports hernias are often misdiagnosed with hip labrum tears, hip impingement, adductor tendonitis and abdominal strains.
Option 1: Groin On-Demand Webinar https://bit.ly/37thtNF
Option 2: eBook Unveiling The Mystery Behind Groin Pain in Athletes https://www.p2sportscare.com/p....roduct/understanding
Option 2: Video Guide https://bit.ly/33aLIqC
Option 3 (the best): Work With Us https://www.p2sportscare.com/
Sports Hernia Diagnosis
What Is A Sports Hernia?
A sports hernia is tearing of the transversalis fascia of the lower abdominal or groin region. A common misconception is that a sports hernia is the same as a traditional hernia. The mechanism of injury is rapid twisting and change of direction within sports, such as football, basketball, soccer and hockey.
The term “sports hernia” is becoming mainstream with more professional athletes being diagnosed. The following are just to name a few:
Torii Hunter
Tom Brady
Ryan Getzlaf
Julio Jones
Jeremy Shockey
If you follow any of these professional athletes, they all seem to have the same thing in common: Lingering groin pain. If you play fantasy sports, this is a major headache since it seems so minor, but it can land a player on Injury Reserve on a moments notice. In real life, it is a very frustrating condition to say the least. It is hard to pin point, goes away with rest and comes back after activity, but is hardly painful enough to make you want to stop. It lingers and is always on your mind. And if you’re looking for my step-by-step sports hernia rehab video course here it is.
One the best definitions of Sport hernias is the following by Harmon:
The phenomena of chronic activity–related groin pain that it is unresponsive to conservative therapy and significantly improves with surgical repair.”
This is truly how sports hernias behave in a clinical setting. It is not uncommon for a sports hernia to be unrecognized for months and even years. Unlike your typical sports injury, most sports medicine offices have only seen a handful of cases. It’s just not on most doctors’ radar. The purpose of this article is not only to bring awareness about sports hernias, but also to educate.
Will you find quick fixes in this article for sports hernia rehab?
Nope. There is no quick fix for this condition, and if someone is trying to sell you one, they are blowing smoke up your you-know-what.
Is there a way to decrease the pain related to sports hernias?
Yes. Proper rehab and avoidance of activity for a certain period of time will assist greatly, but this will not always stop it from coming back. Pain is the first thing to go and last thing to come. Do not be fooled when you become pain-free by resting it. Pain is only one measure of improvement in your rehab. Strength, change of direction, balance and power (just to name a few) are important, since you obviously desire to play your sport again. If you wanted to be a couch potato, you would be feeling better in no time. Watching Sports Center doesn’t require any movement.
Why is this article so long?
There is a lot of information on sports hernias available to you on the web. However, much of the information is spread out all over the internet and hard for athletes to digest due to complicated terminology. This article lays out the foundational terminology you will need to understand what options you have with your injury. We will go over anatomy, biomechanics, rehab, surgery, and even the fun facts. The information I am using is from the last ten years of medical research, up until 2016. We will be making updates overtime when something new is found as well. So link to this page and share with friends. This is the best source for information on sports hernias you will find.
Common Names (or Aliases?) for Sports Hernias
Sportsman’s Hernia
Athletic Pubalgia
Gilmore’s Groin
How Do You Know If You Have A Sports Hernia?
Typical athlete characteristics:
Male, age mid-20s
#sportsherniadiagnosisselftreatment #sportshernia #california

Rotator cuff pain commonly causes local swelling and tenderness in the front of the shoulder. You may have pain and stiffness when you lift your arm. There may also be pain when the arm is lowered from an elevated position. Beginning symptoms may be mild. Patients frequently do not seek treatment at an early stage. These symptoms may include: Minor pain that is present both with activity and at rest Pain radiating from the front of the shoulder to the side of the arm Sudden pain with lifting and reaching movements Athletes in overhead sports may have pain when throwing or serving a tennis ball As the problem progresses, the symptoms increase: Pain at night Loss of strength and motion Difficulty doing activities that place the arm behind the back, such as buttoning or zippering If the pain comes on suddenly, the shoulder may be severely tender. All movement may be limited and painful.

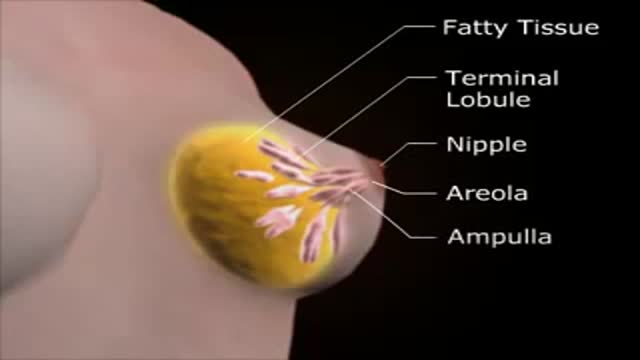
Intrauterine insemination (IUI) is a fertility treatment that involves placing sperm inside a woman's uterus to facilitate fertilization. The goal of IUI is to increase the number of sperm that reach the fallopian tubes and subsequently increase the chance of fertilization
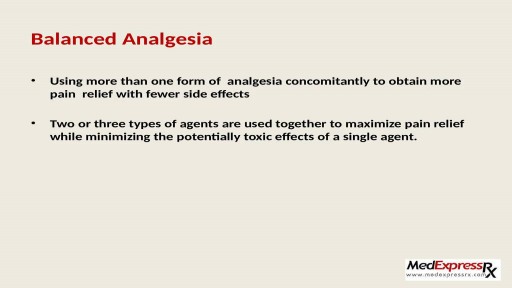
Pain in joints or any part of body is very unpleasant and annoying experience. It is very common in people those suffering from arthritis. To get an end to all such pains, one can start using Generic Celebrex ( https://www.medexpressrx.com/celebrex-generic.aspx ). Here is a brief detail about this wonderful painkiller.