Top videos

Finding a donor heart can be difficult. The heart must be donated by someone who is brain-dead but is still on life support. The donor heart must be matched as closely as possible to your tissue type to reduce the chance that your body will reject it. You are put into a deep sleep with general anesthesia, and a cut is made through the breastbone. Your blood flows through a heart-lung bypass machine while the surgeon works on your heart. This machine does the work of your heart and lungs while they are stopped, and supplies your body with blood and oxygen. Your diseased heart is removed and the donor heart is stitched in place. The heart-lung machine is then disconnected. Blood flows through the transplanted heart, which takes over supplying your body with blood and oxygen. Tubes are inserted to drain air, fluid, and blood out of the chest for several days, and to allow the lungs to fully re-expand.
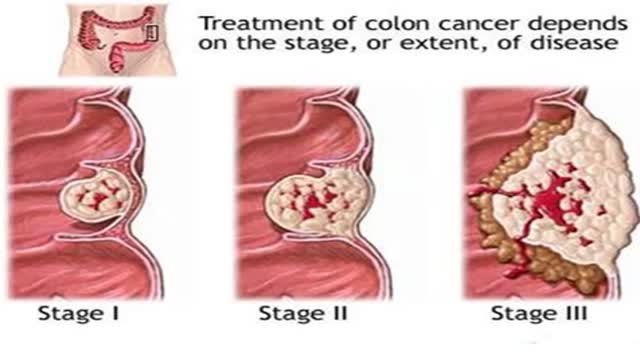
Signs and symptoms of colon cancer include: A change in your bowel habits, including diarrhea or constipation or a change in the consistency of your stool, that lasts longer than four weeks Rectal bleeding or blood in your stool Persistent abdominal discomfort, such as cramps, gas or pain A feeling that your bowel doesn't empty completely Weakness or fatigue Unexplained weight loss Many people with colon cancer experience no symptoms in the early stages of the disease. When symptoms appear, they'll likely vary, depending on the cancer's size and location in your large intestine.
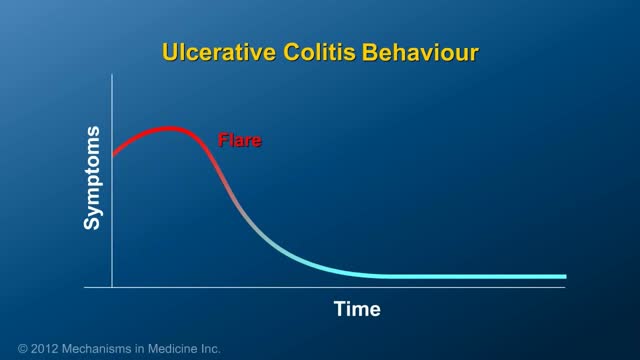
Ulcerative colitis (UL-sur-uh-tiv koe-LIE-tis) is an inflammatory bowel disease (IBD) that causes long-lasting inflammation and ulcers (sores) in your digestive tract. Ulcerative colitis affects the innermost lining of your large intestine (colon) and rectum. Symptoms usually develop over time, rather than suddenly. Ulcerative colitis can be debilitating and sometimes can lead to life-threatening complications. While it has no known cure, treatment can greatly reduce signs and symptoms of the disease and even bring about long-term remission.

In breech position, the baby's bottom is down. There are a few types of breech: Complete breech means the baby is bottom-first, with knees bent. Frank breech means the baby's legs are stretched up, with feet near the head. Footling breech means one leg is lowered over the mother's cervix. You are more likely to have a breech baby if you: Go into early labor Have an abnormally shaped uterus, fibroids, or too much amniotic fluid Have more than one baby in your womb Have placenta previa (when the placenta is on the lower part of the uterine wall, blocking the cervix)

Intrauterine insemination (IUI) is a fertility treatment that involves placing sperm inside a woman's uterus to facilitate fertilization. The goal of IUI is to increase the number of sperm that reach the fallopian tubes and subsequently increase the chance of fertilization

In today's video our patient is on the second stage of her breast reconstruction journey. Previously she had a mastectomy on the left side then we inserted a tissue expander to help stretch the breast tissue to create a pocket for the permanent breast implant that we are placing in today's video. On top of the breast implant we are grafting this patient's own fat into the breast to add a little extra volume and help it be more symmetrical with the other breast.

(cryptorchidism) is a testicle that hasn't moved into its proper position in the bag of skin hanging below the penis (scrotum) before birth. Usually just one testicle is affected, but about 10 percent of the time both testicles are undescended. An undescended testicle is uncommon in general, but common among baby boys born prematurely. The vast majority of the time, the undescended testicle moves into the proper position on its own, within the first few months of life. If your son has an undescended testicle that doesn't correct itself, surgery can relocate the testicle into the scrotum.

Medications are the most proven, effective way to treat gout symptoms. However, making certain lifestyle changes also may help, such as: Limiting alcoholic beverages and drinks sweetened with fruit sugar (fructose). Instead, drink plenty of nonalcoholic beverages, especially water. Limit intake of foods high in purines, such as red meat, organ meats and seafood. Exercising regularly and losing weight. Keeping your body at a healthy weight reduces your risk of gout.
An intrauterine device (IUD), also known as intrauterine contraceptive device (IUCD or ICD) or coil, is a small, often T-shaped birth control device that is inserted into a woman's uterus to prevent pregnancy. IUDs are one form of long-acting reversible birth control (LARC).
Though the risk of HIV transmission through oral sex is very low, but several factors might increase the risk, including sores in the mouth or vagina or on the penis, bleeding gums, having an oral contact with menstrual blood, and the presence of other sexually transmitted diseases. But still the risk is low. by the way better to think twice before having the Oralsex with strangers. because you are not safe 100%.