Top videos

Intestinal malrotation is a developmental anomaly that occasionally causes an unusual array of symptoms in adults. The delay in diagnosis that is common in patients with malrotation frequently results in a ruptured appendix. Appendicitis should be considered when characteristic signs and symptoms are present, even if the location of abdominal pain is atypical.
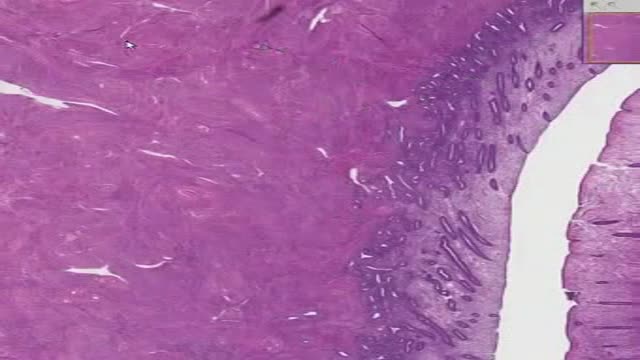
A new natural painkiller based on a body-own molecule, available as supplement. An educational video on its mechanism of action: palmitoylethanolamide (PEA) is a new compound ready 4 use in the clinic to calm glia and mast cells in all states of chronic pain. Thus it focusses on 2 new targets in the treatment of pain: these extra-neuronal targets in chronic pain can be modulated by PEA.
Pancreatitis is inflammation in the pancreas. The pancreas is a long, flat gland that sits tucked behind the stomach in the upper abdomen. The pancreas produces enzymes that assist digestion and hormones that help regulate the way your body processes sugar (glucose). Pancreatitis can occur as acute pancreatitis — meaning it appears suddenly and lasts for days. Or pancreatitis can occur as chronic pancreatitis, which describes pancreatitis that occurs over many years. Mild cases of pancreatitis may go away without treatment, but severe cases can cause life-threatening complications.

Retropharyngeal abscess (RPA) produces the symptoms of sore throat, fever, neck stiffness, and stridor. RPA occurs less commonly today than in the past because of the widespread use of antibiotics for suppurative upper respiratory infections. The incidence of RPA in the United States is rising, however. Once almost exclusively a disease of children, RPA is observed with increasing frequency in adults. It poses a diagnostic challenge for the emergency physician because of its infrequent occurrence and variable presentation.

Proper placement of sutures enhances the precise approximation of the wound edges, which helps minimize and redistribute skin tension. Wound eversion is essential to maximize the likelihood of good epidermal approximation. Eversion is desirable to minimize the risk of scar depression secondary to tissue contraction during healing. Usually, inversion is not desirable, and it probably does not decrease the risk of hypertrophic scarring in an individual with a propensity for hypertrophic scars. The elimination of dead space, the restoration of natural anatomic contours, and the minimization of suture marks are also important to optimize the cosmetic and functional results.

Gonorrhea is a sexually transmitted disease (STD). It’s caused by infection with the bacterium Neisseria gonorrhoeae. It tends to infect warm, moist areas of the body, including the: urethra (the tube that drains urine from the urinary bladder) eyes throat vagina anus female reproductive tract (the fallopian tubes, cervix, and uterus) Gonorrhea passes from person to person through unprotected oral, anal, or vaginal sex. People with numerous sexual partners or those who don’t use a condom are at greatest risk of infection. The best protections against infection are abstinence, monogamy (sex with only one partner), and proper condom usage. Behaviors that make a person more likely to engage in unprotected sex also increase the likelihood of infection. These behaviors include alcohol abuse and illegal drug abuse, particularly intravenous drug use.

A Pap smear (Papanicolau smear; also known as the Pap test) is a screening test for cervical cancer. The test itself involves collection of a sample of cells from a woman's cervix (the end of the uterus that extends into the vagina) during a routine pelvic exam

Urinary incontinence isn't a disease, it's a symptom. It can be caused by everyday habits, underlying medical conditions or physical problems. A thorough evaluation by your doctor can help determine what's behind your incontinence. Temporary urinary incontinence Certain drinks, foods and medications can act as diuretics — stimulating your bladder and increasing your volume of urine. They include: Alcohol Caffeine Decaffeinated tea and coffee Carbonated drinks Artificial sweeteners Corn syrup Foods that are high in spice, sugar or acid, especially citrus fruits Heart and blood pressure medications, sedatives, and muscle relaxants Large doses of vitamins B or C Urinary incontinence also may be caused by an easily treatable medical condition, such as: Urinary tract infection. Infections can irritate your bladder, causing you to have strong urges to urinate, and sometimes incontinence. Other signs and symptoms of urinary tract infection include a burning sensation when you urinate and foul-smelling urine. Constipation. The rectum is located near the bladder and shares many of the same nerves. Hard, compacted stool in your rectum causes these nerves to be overactive and increase urinary frequency. Persistent urinary incontinence Urinary incontinence can also be a persistent condition caused by underlying physical problems or changes, including: Pregnancy. Hormonal changes and the increased weight of the uterus can lead to stress incontinence. Childbirth. Vaginal delivery can weaken muscles needed for bladder control and also damage bladder nerves and supportive tissue, leading to a dropped (prolapsed) pelvic floor. With prolapse, the bladder, uterus, rectum or small intestine can get pushed down from the usual position and protrude into the vagina. Such protrusions can be associated with incontinence. Changes with age. Aging of the bladder muscle can decrease the bladder's capacity to store urine. Menopause. After menopause women produce less estrogen, a hormone that helps keep the lining of the bladder and urethra healthy. Deterioration of these tissues can aggravate incontinence. Hysterectomy. In women, the bladder and uterus are supported by many of the same muscles and ligaments. Any surgery that involves a woman's reproductive system, including removal of the uterus, may damage the supporting pelvic floor muscles, which can lead to incontinence. Enlarged prostate. Especially in older men, incontinence often stems from enlargement of the prostate gland, a condition known as benign prostatic hyperplasia. Prostate cancer. In men, stress incontinence or urge incontinence can be associated with untreated prostate cancer. But more often, incontinence is a side effect of treatments for prostate cancer. Obstruction. A tumor anywhere along your urinary tract can block the normal flow of urine, leading to overflow incontinence. Urinary stones — hard, stone-like masses that form in the bladder — sometimes cause urine leakage. Neurological disorders. Multiple sclerosis, Parkinson's disease, stroke, a brain tumor or a spinal injury can interfere with nerve signals involved in bladder control, causing urinary incontinence.