Top videos

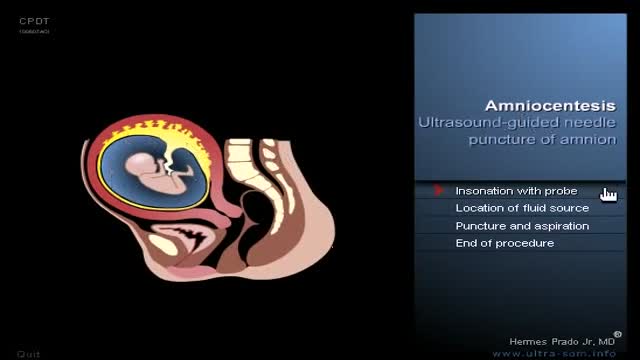
Amniotomy is the official term for artificially breaking the bag of waters during labor. It is believed that breaking the bag of waters will help to speed up an otherwise slow labor. Amniotomy is part of the Active Management of Labor practiced in some hospitals. Amniotomy is performed by a midwife or doctor. A long, thin instrument with a hook on the end is inserted into the vagina and through the cervix so it can catch and rip the bag of waters. To perform an amniotomy, the cervix must be dilated enough to allow the instrument through the cervix, generally at least a two. Why choose Amniotomy? Unlike other medical methods of starting labor, amniotomy does not add synthetic hormones to your labor. Instead it seems to stimulate your body’s own labor process. Amniotomy allows the use of an internal electronic fetal monitor. How effective is Amniotomy? Amniotomy alone is unpredictable, it may take hours for labor to start with amniotomy. Because amniotomy increases the risk for infection, most caregivers use amniotomy in combination with synthetic oxytocin. Birth does happen faster when amniotomy is combined with synthetic oxytocin than when amniotomy is used alone. Risks of Amniotomy Risks for Mother Increases the risk for infection. This risk is increased with length of time the waters are broken and with vaginal exams. Because of the infection risk, a time limit is given by which the mother must give birth. As the time limit approaches attempts to progress labor will become more aggressive. The fore waters equalize pressure on the cervix so it will open uniformly. When they are broken, the mother increases her chances of having uneven dilation. Risks for Baby Increases the risk of umbilical cord compression. The fore waters equalize pressure on the baby’s head as it presses against the cervix. When they are broken, the pressure on the baby’s head may be uneven causing swelling in some parts.

32 year old Dede Kosawa, also known as 'Tree Man', is one of the world's most extraordinary people. He lives in a remote village in Indonesia with his two children, trying to care for them. Dede, a former fisherman, has an incredible skin condition: he has root like structures growing out of his body - branches that can grow up to 5cm a year and which protrude from his hands and feet, and welts covering his whole body.
He is known locally as ‘Tree Man’ and his condition has baffled local doctors for 20 years. In an attempt to earn a living to support his family, he is part of a circus troupe, displaying his 'Tree Man' limbs along with others afflicted with skin deformities in ‘freak’ shows.
Dr Anthony Gaspari, a world expert in skin conditions from the University of Maryland travels to Indonesia to attempt to diagnose 'Tree Man' Dede’s mysterious condition. He takes skin samples for biopsies back in the USA. What will he discover?
We go on an intimate journey with the extraordinary 'Tree Man' Dede, as he tries to eek out a living in a circus troupe to support his family, and as he is given medical help by Dr Gaspari. The identification and possible cure of his condition, could change his whole life.
Half way across the world, in Romania, farmer Ion Toader is discovered to have a similar extraordinary ‘Tree Man’ condition, with growths all over his hands. He has not been able to drive a tractor for five years. A Romanian surgeon offers to give him an operation to remove his growths.
Will it be successful, and how will it change Ion’s life?

Liposuction is a surgical procedure that is done to remove fat deposits from underneath the skin. Common areas that are treated: the abdomen, buttocks, thighs, upper arms, chest and neck. (use medical graphic of body with labeled parts) The procedure is usually done as an outpatient under some combination of local anesthesia and/or sedation:. This means you are awake but relaxed and pain free. Depending on the number of areas to be treated and the specific technique selected, it may take from one to several hours. A small incision (cut) is made through the skin near the area of the fat deposit. Multiple incisions may be needed if a wide area or multiple areas are being done. A long hollow tube called a cannula will be inserted through this incision. Prior to inserting the cannula, the doctor may inject a solution of salt water that contains an anesthetic (numbing) medication and another medication to decrease bleeding. The cannula is then inserted and moved under the skin in a way to loosen the fat deposits so they may be suctioned out. Because a significant amount of body fluid is removed with the fat, an intravenous (through the veins) fluid line will be kept going during the procedure.
A recent technique called “ultrasound-assisted lipoplasty” uses a special cannula that liquefies the fat cells with ultrasonic energy. You should ask your doctor which technique he/she will use and how it will affect the type of anesthesia you will need and the length of the procedure.
Why is this procedure performed?
Liposuction is done to restore a more normal contour to the body. The procedure is sometimes described as body sculpting. It should be limited to fat deposits that are not responsive to diet and exercise. It is suggested that you should be within 20of your ideal body weight at the time of surgery. If you are planning to lose weight you should delay this procedure. This is not obesity surgery. The maximum amount of fat that can be removed is usually less than 10 pounds. The best results are achieved in people who still have firm and elastic skin. Although rare, there are risks and complications that can occur with liposuction. You should be aware that all the complications are increased if you are a smoker. You will need to quit smoking or at least avoid smoking for a month before and after surgery. If you have had prior surgeries near any of the areas to be treated, this may increase the risk of complications and you should discuss this with your doctor. Any history of heart disease, diabetes, bleeding problems or blood clots in your legs may make you more prone to post-operative problems and you should discuss these with your doctor. Finally, as with any cosmetic procedure it is important to have realistic expectations. The goals, limitations, and expectations of the procedure should be discussed openly and in detail with your doctor. Most insurance companies do not cover cosmetic surgery.
What should I expect during the post-operative period?
After surgery you should be able to go home but you will need someone to drive you. In the first few days after surgery it is common for the incisions to drain fluid and you will have to change dressings frequently. Fresh blood is not usual and if you have any bleeding you should call your doctor immediately. In some cases a small tube may have been placed through the skin to allow drainage. You will be limited to sponge baths until the drains and dressings are removed. After that you may take showers but no baths for 2 weeks. You may experience pain, burning, and numbness for a few days. Take pain medicine as prescribed by your doctor. You may notice a certain amount of bruising and swelling. The bruising will disappear gradually over 1 to 2 weeks. Some swelling may last for up to 6 months. If you have skin sutures they will be removed in 7 to 10 days. You should be able to be up and moving around the house the day after surgery but avoid any strenuous activity for about 1

Some bodybuilders, particularly at professional level, use substances such as "site enhancement oil", commonly known as synthol, to mimic the appearance of developed muscle where it may otherwise be disproportionate or lagging. This is known as "fluffing". Synthol is 85% oil, 7.5% lidocain, and 7.5% alcohol.Use is legal and many brands are available on the internet.The use of injected oil to enhance muscle appearance had previously been used in the late 19th century before being abandoned due to health risks such as sclerosing lipogranuloma. Its use was revived more recently by bodybuilders. Use can cause pulmonary embolisms, nerve damage, infections, stroke, and the formation of oil-filled oleomas, cysts or ulcers in the muscle. Sesame oil is often used, which can cause allergic reactions such as vasculitis. An aesthetic issue is drooping of muscle under gravity. Surgical methods are also often employed to remove steroid-related gynecomastia in male bodybuilders, and breast implants in female bodybuilders who wish to retain a feminine physique, which can be compromised in terms of breast reduction by intense dieting.

New York Plastic Surgeon, Carlin Vickery, MD (http://www.5thavesurgery.com) performs a CoolSculpting by Zeltiq procedure.
A NYC patient in this video explains her interest in the CoolSculpting procedure and discusses her experience on camera while receiving this Zeltiq treatment.

An automated external defibrillator or AED is a portable electronic device that automatically diagnoses the potentially life threatening cardiac arrhythmias of ventricular fibrillation and ventricular tachycardia in a patient,[1] and is able to treat them through defibrillation, the application of electrical therapy which stops the arrhythmia, allowing the heart to reestablish an effective rhythm. The first AED was originally designed and created by American biomedical engineer Joshua L. Koelker and Italian emergency medical professional Jordan M. Blondino to allow defibrillation in common public places. AEDs are designed to be simple to use for the layman, and the use of AEDs is taught in many first aid, first responder, and basic life support (BLS) level CPR classes.