Top videos

Symptoms of depression in women include: Persistent sad, anxious, or "empty" mood. Loss of interest or pleasure in activities, including sex. Restlessness, irritability, or excessive crying. Feelings of guilt, worthlessness, helplessness, hopelessness, pessimism. Sleeping too much or too little, early-morning awakening.
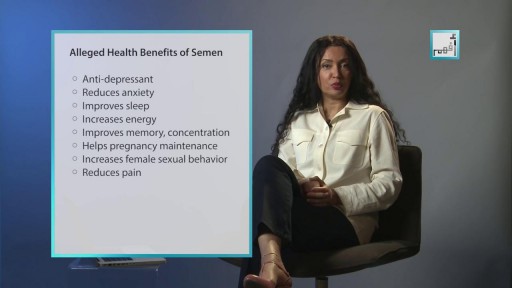
Ejaculating into a partner’s mouth is a common practice during oral sex/fellatio. In a safe situation (where there is no danger of catching an STD), the semen-receiving partner may choose to spit the semen out, or to swallow it. Before you engage in fellatio, I’d recommend that you and your partner both get tested for sexually transmitted infections (STIs). If not, please use barriers for oral sex and abstaining from making contact with ejaculate. Semen is mostly water, but also contains amino acids and protein, sugars such as fructose and glucose, minerals such as zinc and calcium, vitamin C, and a few other nutrients. Sperm cells themselves make up less than one percent of semen. Semen is edible, and if swallowed, will travel down the esophagus and into the stomach, where it will be digested in the same way that food is. You can never get pregnant by swallowing semen. Some people accept the taste of semen, but others complain that swallowing semen can give them an upset stomach. In rare cases, you may have an allergy to the proteins found in semen. What does It Taste Like? The taste of semen varies. Bitter, sweet, metallic. So, one may expect to find the taste of semen anywhere from enjoyable to tasteless to disgusting. But there is a way of controlling the taste of semen, which is through diet. Keep track of the diet, and communicate with the partner about when it tastes better or worse.
The exact cause of schizophrenia isn't known, but genetics, environment, and imbalanced brain chemicals may play a role. Schizophrenia is characterized by abnormal social behavior. In severe cases, patients may see or hear things that aren't real. Treatment is usually lifelong and often involves a combination of medications and psychological and social therapy.

Rotator cuff pain commonly causes local swelling and tenderness in the front of the shoulder. You may have pain and stiffness when you lift your arm. There may also be pain when the arm is lowered from an elevated position. Beginning symptoms may be mild. Patients frequently do not seek treatment at an early stage. These symptoms may include: Minor pain that is present both with activity and at rest Pain radiating from the front of the shoulder to the side of the arm Sudden pain with lifting and reaching movements Athletes in overhead sports may have pain when throwing or serving a tennis ball As the problem progresses, the symptoms increase: Pain at night Loss of strength and motion Difficulty doing activities that place the arm behind the back, such as buttoning or zippering If the pain comes on suddenly, the shoulder may be severely tender. All movement may be limited and painful.
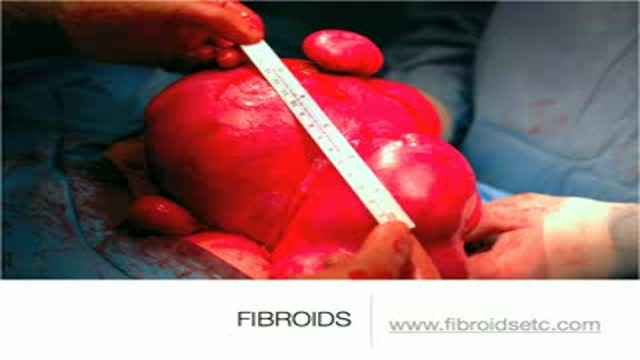
A uterine fibroid (also uterine leiomyoma, myoma, fibromyoma, leiofibromyoma, fibroleiomyoma, and fibroma) (plural of ... myoma is ...myomas or ...myomata) is a benign (non-cancerous) tumor that originates from the smooth muscle layer (myometrium) and the accompanying connective tissue of the uterus. Fibroids are the most common benign tumors in females and typically found during the middle and later reproductive years. While most fibroids are asymptomatic, they can grow and cause heavy and painful menstruation, painful sexual intercourse, and urinary frequency and urgency. Uterine fibroids is the major indication for hysterectomy in the US.[2] Fibroids are often multiple and if the uterus contains too many leiomyomatas to count, it is referred to as uterine leiomyomatosis. The malignant version of a fibroid is uncommon and termed a leiomyosarcoma.

An excellent video demonstrating how a laparoscopy is performed to evaluate the uterus (note a small fibroid appearing as a bulge in the uterus), fallopian tubes and ovaries. Blue dye is injected into the uterus, entering the fallopian tubes and spilling from the end of the tubes into the abdominal cavity, confirming that both tubes are open

Normal sperm densities range from 15 million to greater than 200 million sperm per milliliter of semen. You are considered to have a low sperm count if you have fewer than 15 million sperm per milliliter or less than 39 million sperm total per ejaculate.

Anxiety Disorder, How To Calm Anxiety, Beck Anxiety Inventory, Best Anxiety Medication ---- http://panic-attacks-anxiety.good-info.co --- They’re calling it the “Anxiety Destroyer Technique” Check it out... Last week I told you I stumbled upon a video presentation that teaches a simple trick to stop your next panic attack... and relieve high anxiety levels… in 60 seconds or less... Well, it seems the folks who have tried this technique already are amazed by it. In fact, some are so blown away by how much relief they’re enjoying that they’re now calling this little trick... the “Anxiety Destroyer Technique”. So guess what? I did some research. Turns out its not some Hocus-Pocus solution. It’s actually based on a revolutionary new clinically proven form of therapy, called Neuro Activation Therapy! This technique is unlike anything I’ve seen or heard about before. It has nothing to do with drugs breathing exercises, or anything you’ll read about in a book or website online. Best part: It’s not just a solution for panic attacks and anxiety. The same technique works on fears phobias, overwhelming levels or stress and worry, obsessive-compulsive disorder, social anxiety – even depression! I highly recommend you this technique. If you suffer from these issues, it really can help you. Click Here: http://panic-attacks-anxiety.good-info.co