Top videos

Strep throat is a bacterial infection that can make your throat feel sore and scratchy. Strep throat accounts for only a small portion of sore throats. If untreated, strep throat can cause complications, such as kidney inflammation or rheumatic fever. Rheumatic fever can lead to painful and inflamed joints, a specific type of rash or heart valve damage. Strep throat is most common in children, but it affects people of all ages. If you or your child has signs or symptoms of strep throat, see your doctor for prompt testing and treatment.
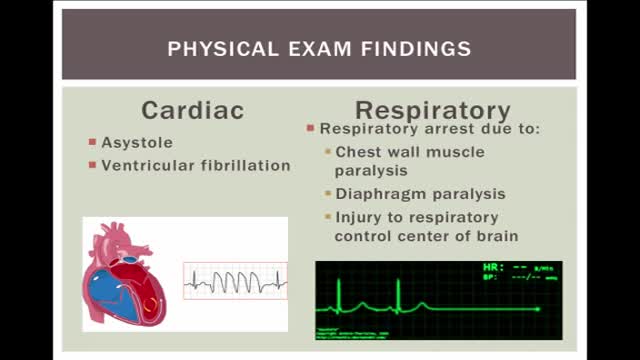
Electrical injuries can present with a variety of problems, including cardiac or respiratory arrest, coma, blunt trauma, and severe burns of several types. It is important to establish the type of exposure (high or low voltage), duration of contact, and concurrent trauma. Low-voltage AC injury without loss of consciousness and/or arrest These injuries are exposures of less than 1000V and usually occur in the home or office setting. Typically, children with electrical injuries present after biting or chewing on an electrical cord and suffer oral burns. Adults working on home appliances or electrical circuits can also experience these electrical injuries. Low-voltage AC may result in significant injury if there is prolonged, tetanic muscle contraction. Low-voltage AC injury with loss of consciousness and/or arrest In respiratory arrest or ventricular fibrillation that is not witnessed, an electrical exposure may be difficult to diagnose. All unwitnessed arrests should include this possibility in the differential diagnosis. Query EMS personnel, family, and coworkers about this possibility. Inquire if a scream was heard before the patient’s collapse; this may be due to involuntary contraction of chest wall muscles from electrical current. High-voltage AC injury without loss of consciousness and/or arrest Usually high-voltage injuries do not cause loss of consciousness but instead cause devastating thermal burns. In occupational exposures, details of voltage can be obtained from the local power company. High-voltage AC injury with loss of consciousness and/or arrest This is an unusual presentation of high-voltage AC injuries, which do not often cause loss of consciousness. History may need to come from bystanders or EMS personnel. Direct current (DC) injury These injuries typically cause a single muscle contraction that throws the victim away from the source. They are rarely associated with loss of consciousness unless there is severe head trauma, and victims can often provide their own history. Conducted electrical devices Conducted electrical weapons (CEWs) such as tasers are weapons used by law enforcement that deliver high-voltage current that is neither true AC or DC but is most like a series of low-amplitude DC shocks.[16] They can deliver 50,000 V in a 5-second pulse, with an average current of 2.1 mA.[17] Though they have been temporally associated with deaths in the law enforcement setting, conducted electrical devices (CEDs) in healthy volunteers have been shown to be safe without evidence of delayed arrhythmia or cardiac damage as measured by troponin I.[18, 17] One study of their use in 1201 law enforcement incidents showed mostly superficial puncture wounds from the device probes, and significant injuries only from trauma subsequent to shock, not from the device itself. Of 2 deaths in custody, neither was related to CEW exposure.[19]
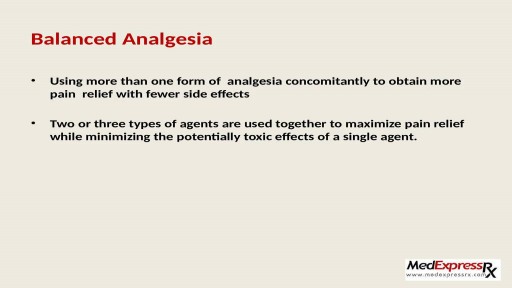
Pain in joints or any part of body is very unpleasant and annoying experience. It is very common in people those suffering from arthritis. To get an end to all such pains, one can start using Generic Celebrex ( https://www.medexpressrx.com/celebrex-generic.aspx ). Here is a brief detail about this wonderful painkiller.

If you have an active lifestyle or are often on the go with work, travel or family, then peritoneal dialysis at home may be the right choice. Home peritoneal dialysis offers additional freedom and flexibility as a treatment option that’s closest to natural kidney function and may require fewer dietary restrictions and medications. To learn more about Home PD, visit https://www.FreseniusKidneyCar....e.com/ckd-treatment/
Subscribe to Our YouTube Channel
Subscribe Here: https://www.youtube.com/c/Fres....eniusKidneyCareOffic
Find Fresenius Kidney Care Online at:
Website: https://www.freseniuskidneycare.com/
Facebook:@FreseniusKidneyCare
https://www.facebook.com/FreseniusKidneyCare/
Twitter: @FreseniusKC
https://twitter.com/freseniuskc
Pinterest: Fresenius Kidney Care
https://www.pinterest.com/FreseniusKidneyCarePins/

Causes are chronic inflammation due to infection, allergies, drug sensitivity, or immune disorders. Symptoms may include a runny nose, stuffiness, or post-nasal drip. In some cases, there may be no symptoms. The condition can be treated with corticosteroids, other medications, or surgery.
PKU is inherited in families in an autosomal recessive pattern. Autosomal recessive inheritance means that a person has two copies of the gene that is altered. Usually, each parent of an individual who has PKU carries one copy of the altered gene. ... Gene alterations (mutations) in the PAH gene cause PKU.

An excellent video demonstrating how a laparoscopy is performed to evaluate the uterus (note a small fibroid appearing as a bulge in the uterus), fallopian tubes and ovaries. Blue dye is injected into the uterus, entering the fallopian tubes and spilling from the end of the tubes into the abdominal cavity, confirming that both tubes are open