Top videos
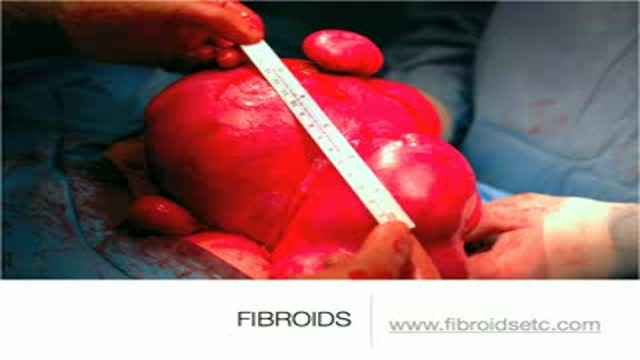
A uterine fibroid (also uterine leiomyoma, myoma, fibromyoma, leiofibromyoma, fibroleiomyoma, and fibroma) (plural of ... myoma is ...myomas or ...myomata) is a benign (non-cancerous) tumor that originates from the smooth muscle layer (myometrium) and the accompanying connective tissue of the uterus. Fibroids are the most common benign tumors in females and typically found during the middle and later reproductive years. While most fibroids are asymptomatic, they can grow and cause heavy and painful menstruation, painful sexual intercourse, and urinary frequency and urgency. Uterine fibroids is the major indication for hysterectomy in the US.[2] Fibroids are often multiple and if the uterus contains too many leiomyomatas to count, it is referred to as uterine leiomyomatosis. The malignant version of a fibroid is uncommon and termed a leiomyosarcoma.

Antisocial personality disorder (ASPD) is defined by the American Psychiatric Association's Axis II (personality disorders) of the Diagnostic and Statistical Manual (DSM-IV-TR) as "a pervasive pattern of disregard for, and violation of, the rights of others that begins in childhood or early adolescence and continues into adulthood." Antisocial personality disorder is sometimes wrongly referred to as psychopathy or sociopathy. Currently, neither psychopathy nor sociopathy are valid diagnoses described in the Diagnostic and Statistical Manual of Mental Disorders, and the ICD-10 of the World Health Organization also lacks psychopathy as a diagnostic disorder. Psychopathy is normally seen as a subset of the antisocial personality disorder, but Blair believes that the antisocial personality disorder and psychopathy may be separate conditions altogether.

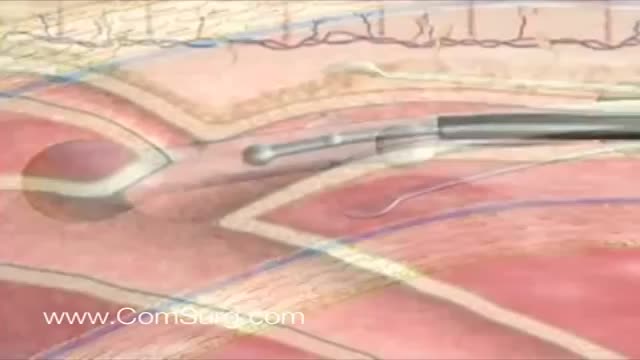
An excellent video demonstrating how a laparoscopy is performed to evaluate the uterus (note a small fibroid appearing as a bulge in the uterus), fallopian tubes and ovaries. Blue dye is injected into the uterus, entering the fallopian tubes and spilling from the end of the tubes into the abdominal cavity, confirming that both tubes are open

To avoid pregnancy and STDs, always remember to use a condom every time you have sex — including oral, vaginal, or anal sex. Whenever oral sex is being performed on a girl, a dental dam should be used. A guy receiving oral sex should wear a latex condom — or, if he or his partner is allergic to latex, a polyurethane condom.

James Slover, MD, and Ivan Madrid, MD, describe the benefits of knee replacement surgery, the differences in partial and total knee replacement, and how the procedures are performed at NYU Langone.
Learn more about Dr. Slover: http://nyulangone.org/doctors/....1851355564/james-d-s
Learn more about Dr. Madrid: http://nyulangone.org/doctors/....1912940107/ivan-madr
To learn more about joint replacement surgery at NYU Langone, visit: http://nyulangone.org/location....s/center-for-musculo

Symptoms of depression in women include: Persistent sad, anxious, or "empty" mood. Loss of interest or pleasure in activities, including sex. Restlessness, irritability, or excessive crying. Feelings of guilt, worthlessness, helplessness, hopelessness, pessimism. Sleeping too much or too little, early-morning awakening.

St. Luke's originally broadcast this live in a webcast and later re-purposed it for air on KCRG-TV9 as an educational video. It is hosted by Ashley Hinson, KCRG-TV9 anchor and Dr. Sandeep Munjal. Dr. Jeff Nassif performs the knee replacement surgery on an eastern Iowa woman. St. Luke's has a rapid recovery joint replacement program, which gets people back to life quickly after surgery.

After the cell membranes are dissolved, the typical branching and budding yeast cells can be seen. Sometimes, it has the appearance of a tangled web of threads. At other times, only small branches will be seen.Yeast are normal inhabitants of the vagina, but only in very small numbers. If you visualize any yeast in your sample, it is considered significant.

Paracentesis is a procedure to take out fluid that has collected in the belly (peritoneal fluid). This fluid buildup is called ascites . Ascites may be caused by infection, inflammation, an injury, or other conditions, such as cirrhosis or cancer. The fluid is taken out using a long, thin needle put through the belly.

Rhabdomyolysis is a condition in which damaged skeletal muscle (Ancient Greek: rhabdomyo-) tissue breaks down rapidly (Greek –lysis). This damage may be caused by physical (e.g. crush injury), chemical, or biological factors. Breakdown products of damaged muscle cells are released into the bloodstream; some of these, such as the protein myoglobin, are harmful to the kidney and may lead to kidney dysfunction. The severity of the symptoms (which may include muscle pains, vomiting and confusion) depends on the extent of the muscle damage, and whether kidney failure develops. The mainstay of treatment is generous intravenous fluids, but could include dialysis or hemofiltration.
Rhabdomyolysis and its complications are significant problems for those injured in disasters such as earthquakes and bombing. Relief efforts in areas struck by earthquakes often include medical teams with skills and equipment for treatment of survivors with rhabdomyolysis. The disease and its mechanisms were first fully elucidated during the Blitz of London in 1941.
Like the VenaCure EVLT® procedure, which uses a laser to ablate the varicose vein, VNUS RF treatment is an alternative to more invasive leg stripping surgery. It is used primarily to treat the great saphenous veins (GSV), small saphenous vein (SSV), and other superficial veins in the legs.