Top videos
The Epley maneuver is a series of movements, normally carried out on a person by a doctor, to relieve the symptoms of BPPV. Research has found it to be an easy, safe, and effective treatment for the condition in both the long- and short-term. The Epley maneuver is sometimes called the particle repositioning maneuver or the canalith repositioning maneuver. These names are used because the maneuver involves a series of movements that help to reposition crystals in a person's ear that may cause feelings of dizziness. Repositioning the crystals helps to relieve the person's dizziness and nausea.

LIS Closed done at 5 O clock position, using Scalpel blade 15. After feeling the groove between internal and external anal sphincter, the blade is passed in and the lower 1/2 of Internal anal sphincter is cut. Remain below dentate line. If anal mucosa is accidently cut suture with 4-0 rapid vicryl. In event of bleeding, pinchcock for 5 minutes.
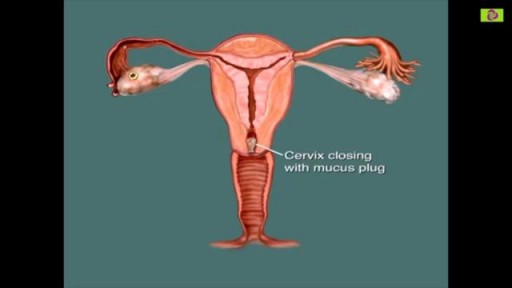
You are most fertile at the time of ovulation, (when an egg is released from your ovaries) which usually occurs 12-14 days before your next period starts. This is the time of the month when you are most likely to get pregnant. It is unlikely that you will get pregnant just after your period, although it can happen.

A coma is a prolonged state of unconsciousness. During a coma, a person is unresponsive to his or her environment. The person is alive and looks like he or she is sleeping. However, unlike in a deep sleep, the person cannot be awakened by any stimulation, including pain.

Pyogenic liver abscesses are mainly treated by percutaneous aspiration or drainage under antibiotic cover. If interventional radiology fails, surgical drainage becomes necessary. Recently, we performed laparoscopic liver abscess drainage successfully, and we aimed to focus on the topic in light of a systematic review of the literature.
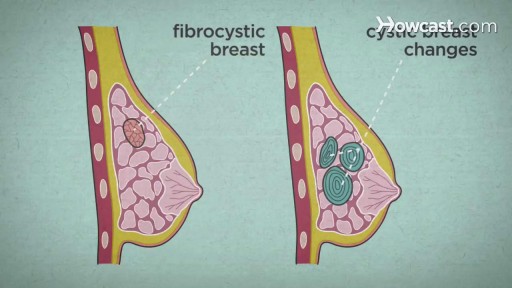
Over the course of a woman's lifetime, she may experience breast changes. While many end up being nothing to worry about, it's important to have any changes that you notice checked by a doctor -- just to be on the safe side. Here are the potential breast cancer symptoms to watch out for.
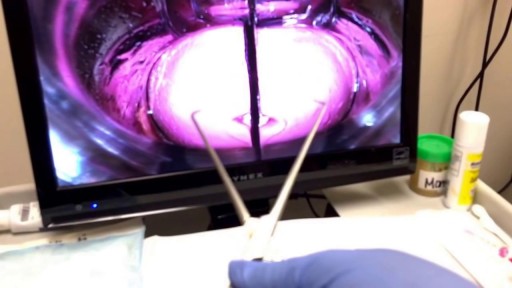
An intrauterine device (IUD), also known as intrauterine contraceptive device (IUCD or ICD) or coil, is a small, often T-shaped birth control device that is inserted into a woman's uterus to prevent pregnancy. IUDs are one form of long-acting reversible birth control (LARC).

• Define and use related medical terminology.
• Describe and demonstrate techniques for imaging the thyroid gland.
• Discuss functional abnormalities of the thyroid gland.
• Correlate laboratory data relevant to the thyroid and parathyroid glands.
• Describe, and recognize on images, pathologies of the thyroid gland.
• Identify the anatomy of the parathyroid glands on diagrams and sonograms.
• Describe and demonstrate techniques for imaging the parathyroid glands.
• Describe, and recognize on images, pathologies of the parathyroid glands.
• List and describe other neck masses.
• Follow relevant protocols when scanning.
• Differentiate the sonographic appearances of the female reproductive organs in relation to the menstrual cycle, the use of contraceptives and hormone replacement, and following chemotherapy.
• Explain the Patient Privacy Rule (HIPAA) and Patient Safety Act (see reference).
Given the success of drugs to treat erectile dysfunction, such as sildenafil (Viagra), tadalafil (Cialis) and vardenafil (Levitra), drug companies have sought a comparable drug for women. Viagra has even been tried as a treatment for sexual dysfunction in women. However, the Food and Drug Administration (FDA) hasn't approved this use of Viagra. Indeed, until recently there were no FDA-approved drugs for treating sexual arousal or sexual desire problems in women. Yet 4 in 10 women report having sexual concerns. A prescription medication known as flibanserin (Addyi) — originally developed as an antidepressant — has been approved by the FDA as a treatment for low sexual desire in premenopausal women. A daily pill, Addyi may boost sex drive in women with low sexual desire and who find the experience distressing. Potentially serious side effects include low blood pressure, dizziness and fainting, particularly if the drug is mixed with alcohol. Experts recommend that you stop taking the drug if you don't notice an improvement in your sex drive after eight weeks.