Top videos

Glomus tumors are rare soft tissue neoplasms that typically present in adults (ages 20-40 years) as small, blue-red papules or nodules of the distal extremities, with most cases involving subungual sites. These tumors are typically painful, often causing paroxysmal pain in response to temperature changes or pressure. Glomus tumors are thought to arise from the glomus body, a thermoregulatory shunt concentrated in the fingers and toes. Most lesions are solitary and localized to cutaneous sites; however, generalized glomuvenous malformations, or multiple glomangiomas, have also been described, and may have extracutaneous involvement.
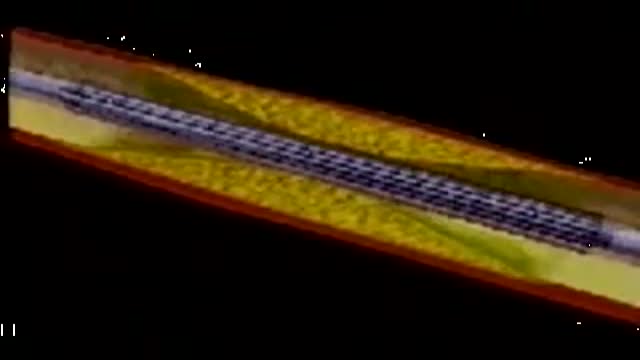
This video depicts how a stent is placed in the coronary artieries. We first place a guiding wire in the heart artery through a catheter, usually from the groin. Then the stent is inflated by a balloon in the artery, which is then removed. The stent remains permanently. Blood thinners, aspirin and plavix, are both required after a stent is placed in your heart artery.

How to improve your eyesight at home? Exercising your eyes is one of those simple things that very few people do. However, it can help you maintain excellent vision. Here are 10 exercises that will take you no more than ten minutes to do. You can give them a try right now while watching this video – we are going to do all of them with you! Exercise #1. Blink for a minute. Exercise #2. Rotate your head while staring ahead. Exercise #3. Look to your right and left. Exercise #4. Close your eyes and relax. Exercise #5. Move your gaze in different directions. Exercise #6. Close and open your eyes. Exercise #7. Push against your temples with your fingers. Exercise #8. Draw geometric figures with your gaze. Exercise #9. Move your eyeballs up and down. Exercise #10. Strengthen your eyes’ near and far focusing.

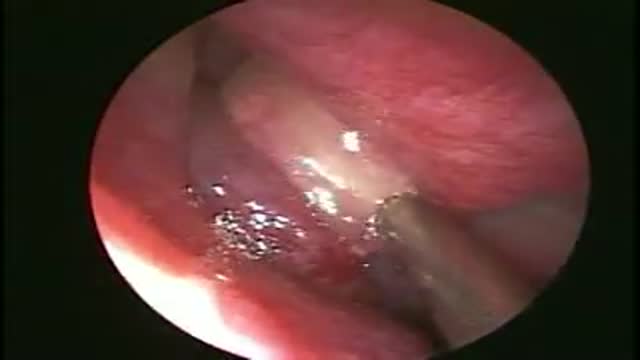
A meningioma is a tumor that arises from the meninges — the membranes that surround your brain and spinal cord. Most meningiomas are noncancerous (benign), though rarely a meningioma may be cancerous (malignant). Some meningiomas are classified as atypical, meaning they're neither benign nor malignant but, rather, something in between.
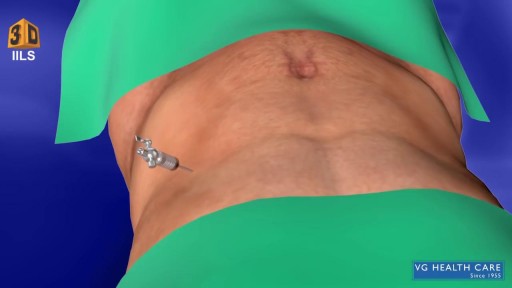
What Is an Appendectomy? An appendectomy is the surgical removal of the appendix. It’s a common emergency surgery that’s performed to treat appendicitis, an inflammatory condition of the appendix. The appendix is a small, tube-shaped pouch attached to your large intestine. It’s located in the lower right side of your abdomen. The exact purpose of the appendix isn’t known. However, it’s believed that it may help us recover from diarrhea, inflammation, and infections of the small and large intestines. These may sound like important functions, but the body can still function properly without an appendix. When the appendix becomes inflamed and swollen, bacteria can quickly multiply inside the organ and lead to the formation of pus. This buildup of bacteria and pus can cause pain around the belly button that spreads to the lower right section of the abdomen. Walking or coughing can make the pain worse. You may also experience nausea, vomiting, and diarrhea. It’s important to seek treatment right away if you’re having symptoms of appendicitis. When the condition goes untreated, the appendix can burst (perforated appendix) and release bacteria and other harmful substances into the abdominal cavity. This can be life-threatening, and will lead to a longer hospital stay. Appendectomy is the standard treatment for appendicitis. It’s crucial to remove the appendix right away, before the appendix can rupture. Once an appendectomy is performed, most people recover quickly and without complications. Why Is an Appendectomy Performed? An appendectomy is often done to remove the appendix when an infection has made it inflamed and swollen. This condition is known as appendicitis. The infection may occur when the opening of the appendix becomes clogged with bacteria and stool. This causes your appendix to become swollen and inflamed. The easiest and quickest way to treat appendicitis is to remove the appendix. Your appendix could burst if appendicitis isn’t treated immediately and effectively. If the appendix ruptures, the bacteria and fecal particles within the organ can spread into your abdomen. This may lead to a serious infection called peritonitis. You can also develop an abscess if your appendix ruptures. Both are life-threatening situations that require immediate surgery. Symptoms of appendicitis include: stomach pain that starts suddenly near the belly button and spreads to the lower right side of the abdomen abdominal swelling rigid abdominal muscles constipation or diarrhea nausea vomiting loss of appetite low-grade fever Although pain from appendicitis typically occurs in the lower right side of the abdomen, pregnant women may have pain in the upper right side of the abdomen. This is because the appendix is higher during pregnancy. Go to the emergency room immediately if you believe you have appendicitis. An appendectomy needs to be performed right away to prevent complications. What Are the Risks of an Appendectomy? An appendectomy is a fairly simple and common procedure. However, there are some risks associated with the surgery, including: bleeding infection injury to nearby organs blocked bowels It’s important to note that the risks of an appendectomy are much less severe than the risks associated with untreated appendicitis. An appendectomy needs to be done immediately to prevent abscesses and peritonitis from developing. How Do I Prepare for an Appendectomy? You’ll need to avoid eating and drinking for at least eight hours before the appendectomy. It’s also important to tell your doctor about any prescription or over-the-counter medications you’re taking. Your doctor will tell you how they should be used before and after the procedure. You should also tell your doctor if you: are pregnant or believe you may be pregnant are allergic or sensitive to latex or certain medications, such as anesthesia have a history of bleeding disorders You should also arrange for a family member or friend to drive you home after the procedure. An appendectomy is often performed using general anesthesia, which can make you drowsy and unable to drive for several hours after surgery. Once you’re at the hospital, your doctor will ask you about your medical history and perform a physical examination. During the exam, your doctor will gently push against your abdomen to pinpoint the source of your abdominal pain. Your doctor may order blood tests and imaging tests if appendicitis is caught early. However, these tests may not be performed if your doctor believes an emergency appendectomy is necessary. Before the appendectomy, you’ll be hooked up to an IV so you can receive fluids and medication. You’ll likely be put under general anesthesia, which means you’ll be asleep during surgery. In some cases, you’ll be given local anesthesia instead. A local anesthetic numbs the area, so even though you’ll be awake during the surgery, you won’t feel any pain. How Is an Appendectomy Performed? There are two types of appendectomy: open and laparoscopic. The type of surgery your doctor chooses depends on several factors, including the severity of your appendicitis and your medical history. Open Appendectomy During an open appendectomy, a surgeon makes one incision in the lower right side of your abdomen. Your appendix is removed and the wound is closed with stiches. This procedure allows your doctor to clean the abdominal cavity if your appendix has burst. Your doctor may choose an open appendectomy if your appendix has ruptured and the infection has spread to other organs. It’s also the preferred option for people who have had abdominal surgery in the past. Laparoscopic Appendectomy During a laparoscopic appendectomy, a surgeon accesses the appendix through a few small incisions in your abdomen. A small, narrow tube called a cannula will then be inserted. The cannula is used to inflate your abdomen with carbon dioxide gas. This gas allows the surgeon to see your appendix more clearly. Once the abdomen is inflated, an instrument called a laparoscope will be inserted through the incision. The laparoscope is a long, thin tube with a high-intensity light and a high-resolution camera at the front. The camera will display the images on a screen, allowing the surgeon to see inside your abdomen and guide the instruments. When the appendix is found, it will be tied off with stiches and removed. The small incisions are then cleaned, closed, and dressed. Laparoscopic surgery is usually the best option for older adults and people who are overweight. It has fewer risks than an open appendectomy procedure, and generally has a shorter recovery time. What Happens After an Appendectomy? When the appendectomy is over, you’ll be observed for several hours before you’re released from the hospital. Your vital signs, such your breathing and heart rate, will be monitored closely. Hospital staff will also check for any adverse reactions to the anesthesia or the procedure. The timing of your release will depend on: your overall physical condition the type of appendectomy performed your body’s reaction to the surgery In some cases, you may have to remain in the hospital overnight. You may be able to go home the same day as the surgery if your appendicitis wasn’t severe. A family member or friend will need to drive you home if you received general anesthesia. The effects of general anesthesia usually take several hours to wear off, so it can be unsafe to drive after the procedure. In the days following the appendectomy, you may feel moderate pain in the areas where incisions were made. Any pain or discomfort should improve within a few days. Your doctor may prescribe medication to relieve the pain. They might also prescribe antibiotics to prevent an infection after surgery. You can further reduce your risk for infection by keeping the incisions clean. You should also watch for signs of infection, which include: redness and swelling around the incision fever above 101°F chills vomiting loss of appetite stomach cramps diarrhea or constipation that lasts for more than two days Although there’s a small risk of infection, most people recover from appendicitis and an appendectomy with little difficulty. Full recovery from an appendectomy takes about four to six weeks. During this time, your doctor will probably recommend that you limit physical activity so your body can heal. You’ll need to attend a follow-up appointment with your doctor within two to three weeks after the appendectomy.
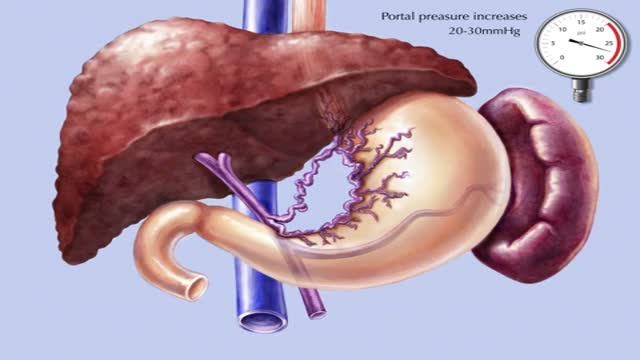
Transjugular intrahepatic portosystemic shunt or transjugular intrahepatic portosystemic stent shunting (commonly abbreviated as TIPS or TIPSS) is an artificial channel within the liver that establishes communication between the inflow portal vein and the outflow hepatic vein.

The peroneal artery is closely positioned to the fibula. The artery arises from the tibioperoneal trunk, distal to the takeoff of the anterior tibial artery (seen in the illustration below perforating the interosseous membrane). The peroneal artery sends perforators laterally to the skin of the lower leg, sometimes in a septocutaneous fashion via the lateral intermuscular septum, but often with muscular perforators. The length of the pedicle is usually short, but can be increased substantially by dissecting the peroneal artery and its venae from the fibula and using the distal bone for reconstruction.

After Sammyra’s knee injury, Marvin Smith, MD, orthopaedic surgeon at Memorial Sports Medicine Center, helped her get back on the volleyball court and playing pain free. Following a thorough examination, meniscus surgery and rehabilitation got Sammyra back to playing with her college team within two months. Learn more about how Memorial Sports Medicine Center helps athletes move forward at MHS.net/SportsMedicine.
To learn more about Dr. Smith, visit his physician profile page at: https://www.mhs.net/physicians/s/smith-marvin-k