Top videos
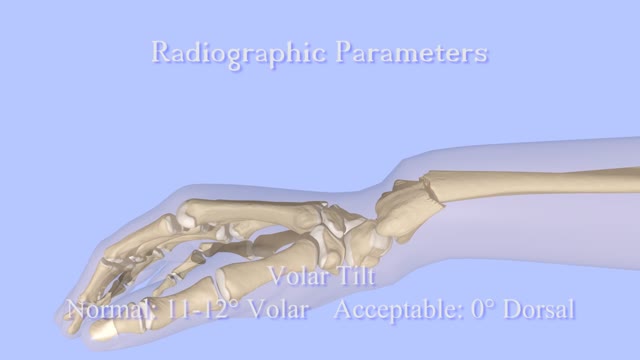
Closed Reduction of Distal Radius Fractures - Discussion: (distal radius fracture menu) - closed reduction & immobilization in plaster cast remains accepted method of treatment for majority of stable distal radius frx; - unstable fractures will often lose reduction in the cast and will slip back to the pre-reduction position; - patients should be examined for carpal tunnel symptoms before and after reduction; - carpal tunnel symptoms that do not resolve following reduction will require carpal tunnel release; - cautions: - The efficacy of closed reduction in displaced distal radius fractures. - Technique: - anesthesia: (see: anesthesia menu) - hematoma block w/ lidocaine; - w/ hematoma block surgeon should look for "flash back" of blood from hematoma, prior to injection; - references: - Regional anesthesia preferable for Colles' fracture. Controlled comparison with local anesthesia. - Neurological complications of dynamic reduction of Colles' fractures without anesthesia compared with traditional manipulation after local infiltration anesthesia. - methods of reduction: - Jones method: involves increasing deformity, applying traction, and immobilizing hand & wrist in reduced position; - placing hand & wrist in too much flexion (Cotton-Loder position) leads to median nerve compression & stiff fingers; - Bohler advocated longitudinal traction followed by extension and realignment; - consider hyper-extending the distal fragment, and then translating it distally (while in extended position) until it can be "hooked over" proximal fragment; - subsequently, the distal fragment can be flexed (or hinged) over the proximal shaft fragment; - closed reduction of distal radius fractures is facilitated by having an assistant provide counter traction (above the elbow) while the surgeon controls the distal fragment w/ both hands (both thumbs over the dorsal surface of the distal fragment); - flouroscopy: - it allows a quick, gentle, and complete reduction; - prepare are by prewrapping the arm w/ sheet cotton and have the plaster or fibroglass ready; - if flouroscopy is not available, then do not pre-wrap the extremity w/ cotton; - it will be necessary to palpate the landmarks (outer shaped of radius, radial styloid, and Lister's tubercle, in order to judge success of reduction; - casting: - generally, the surgeon will use a pre-measured double sugar sugar tong splint, which is 6-8 layers in thickness; - more than 8 layers of plaster can cause full thickness burns: - reference: Setting temperatures of synthetic casts. - position of immobilization - follow up: - radiographs: - repeat radiographs are required weekly for 2-3 weeks to ensure that there is maintenance of the reduction; - a fracture reduction that slips should be considered to be unstable and probably require fixation with (pins, or ex fix ect.) - there is some evidence that remanipulation following fracture displacement in cast is not effective for these fractures; - ultimately, whether or not a patient is satisfied with the results of non operative treatment depends heavily on th

After Sammyra’s knee injury, Marvin Smith, MD, orthopaedic surgeon at Memorial Sports Medicine Center, helped her get back on the volleyball court and playing pain free. Following a thorough examination, meniscus surgery and rehabilitation got Sammyra back to playing with her college team within two months. Learn more about how Memorial Sports Medicine Center helps athletes move forward at MHS.net/SportsMedicine.
To learn more about Dr. Smith, visit his physician profile page at: https://www.mhs.net/physicians/s/smith-marvin-k
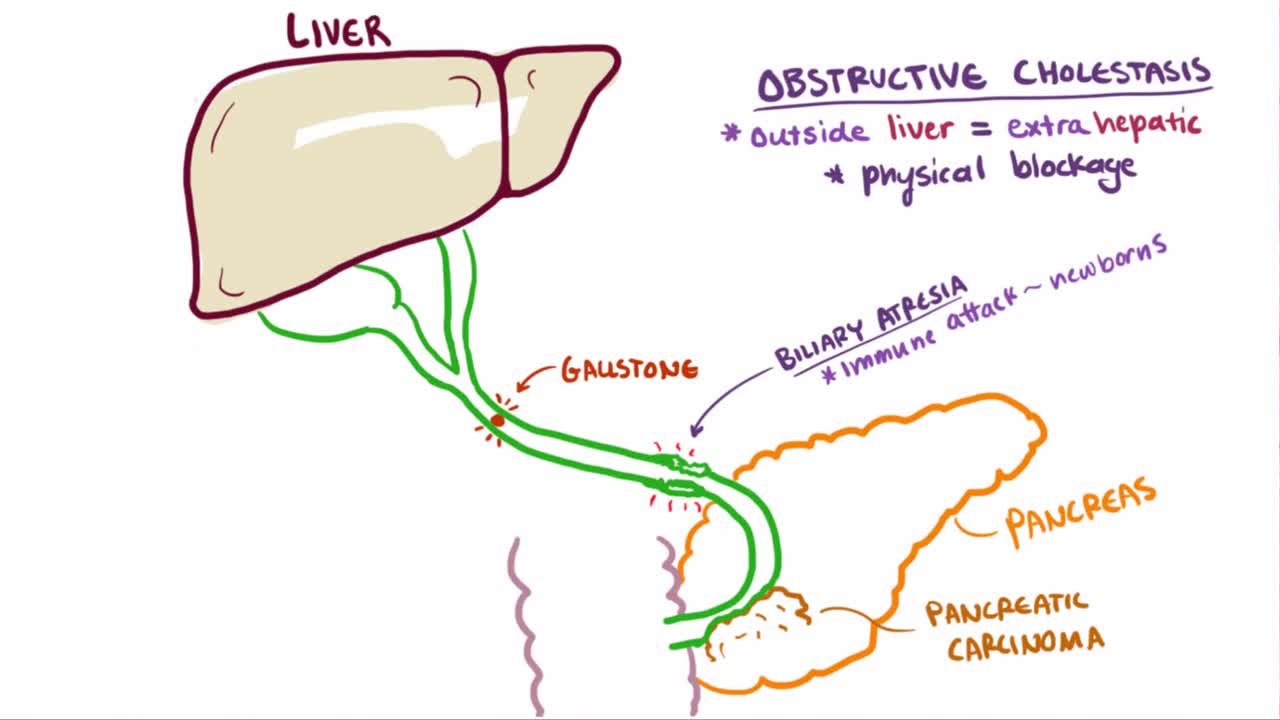
Cholestatic liver disease is a condition that results from an impairment of bile formation or bile flow to the gallbladder and duodenum (first section of the small intestine). ... The effects of cholestasis are profound and widespread, leading to worsening liver disease and systemic illness.

Femoral Embolectomy. Back. All emboli of the lower extremity, including a proximal saddle embolus at the aortic bifurcation, can be removed through the common femoral artery using Fogarty catheters. By passing these through the embolus, and by inflating the small balloon, the clot can be withdrawn and the flow restored

A recap of Mater Hospital patient Helen's story as she progressed from experiencing chronic knee pain due to osteoarthritis, through to knee replacement treatment and ultimately a new lease on life.
Dedicated to surgical excellence and patient-centred care, the Mater Hospital North Sydney is regarded as a leading orthopaedic hospital and the only Australian hospital to be accepted into the International Society of Orthopaedic Centres.
For more information, click here: https://bit.ly/3bvhY8G

Genital warts are soft growths that appear on the genitals. Genital warts are a sexually transmitted infection (STI) caused by certain strains of the human papillomavirus (HPV). These skin growths can cause pain, discomfort, and itching. They are especially dangerous for women because some types of HPV can also cause cancer of the cervix and vulva.

Perdre Du Ventre, Comment Maigrir Des Cuisses, Regime Soupe, Prendre Du Muscle, Maigrir Des Hanches ---- http://perte-poids-rapide.info-pro.co --- Comment maigrir pour un homme ? Les régimes ne sont pas une exclusivité féminine et les hommes ont eux aussi des comptes à rendre à leur balance. Pour séduire, pour se sentir mieux dans leur corps, pour leur travail, ils ont eux aussi des raisons pour se délester de quelques kilos. Hommes et femmes : différentes face aux kilos Les hommes et les femmes ne réagissent pas de la même manière face au poids. Le corps non plus. La première différence est au niveau de la silhouette. La gente féminine va accumuler les kilos en trop au niveau des fesses et des cuisses alors que pour les hommes, la prise de poids se situe surtout au niveau du visage, du cou et du ventre. L’autre différence entre les hommes et les femmes est la faculté à perdre du poids. Si vous avez décidé de suivre un régime en couple, sachez Mesdames que les hommes maigrissent plus vite ! Cette « injustice » est expliquée par le fait que les hommes ou plutôt leur organisme, va brûler plus de calories au repos et à l’effort que les femmes grâce à leur masse corporelle plus importante. Par contre, ces dames sont plus motivées à tenir un régime sur la longueur. Les hommes et les régimes, c’est toute une histoire ! C’est pourquoi ils doivent faire un régime qui leur corresponde et qui est adapté à leur vie au quotidien ! Maigrir lorsque l’on est un homme Les hommes sont de plus en plus nombreux à vouloir perdre du poids. Surtout entre 40 et 45 ans. Mais même s’ils maigrissent plus vite que les femmes, la partie est loin d’être gagnée. Pourquoi ? Parce qu’il est plus compliqué pour eux de modifier leurs habitudes alimentaires. En effet, ce sont les vrais champions d’une alimentation riche en matières grasses, peu variée et très déséquilibrée. Il faut donc qu’ils adoptent de nouvelles habitudes alimentaires tout en conservant une certaines notion de plaisir et qu’ils combattent certaines mauvaises habitudes, souvent responsable de leurs kilos en trop. "Découvrez comment jean-jacques a réussi à perdre 3,2 kilos et 7 cm de tour de taille en 2 semaines, sans peser les aliments ni compter les calories." Cliquez ici: http://perte-poids-rapide.info-pro.co

Pulmonary edema is usually caused by a heart condition. Other causes include pneumonia, exposure to certain toxins and drugs, and being at high elevations. Depending on the cause, pulmonary edema symptoms may appear suddenly or develop over time. Mild to extreme breathing difficulty can occur. Cough, chest pain, and fatigue are other symptoms. Treatment generally includes supplemental oxygen and medications.