Top videos
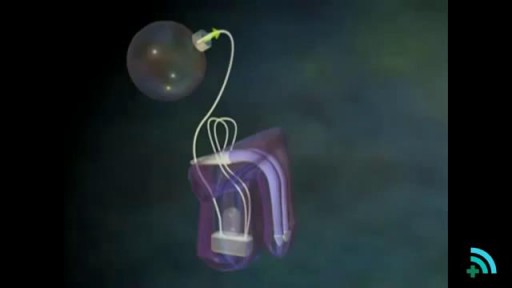
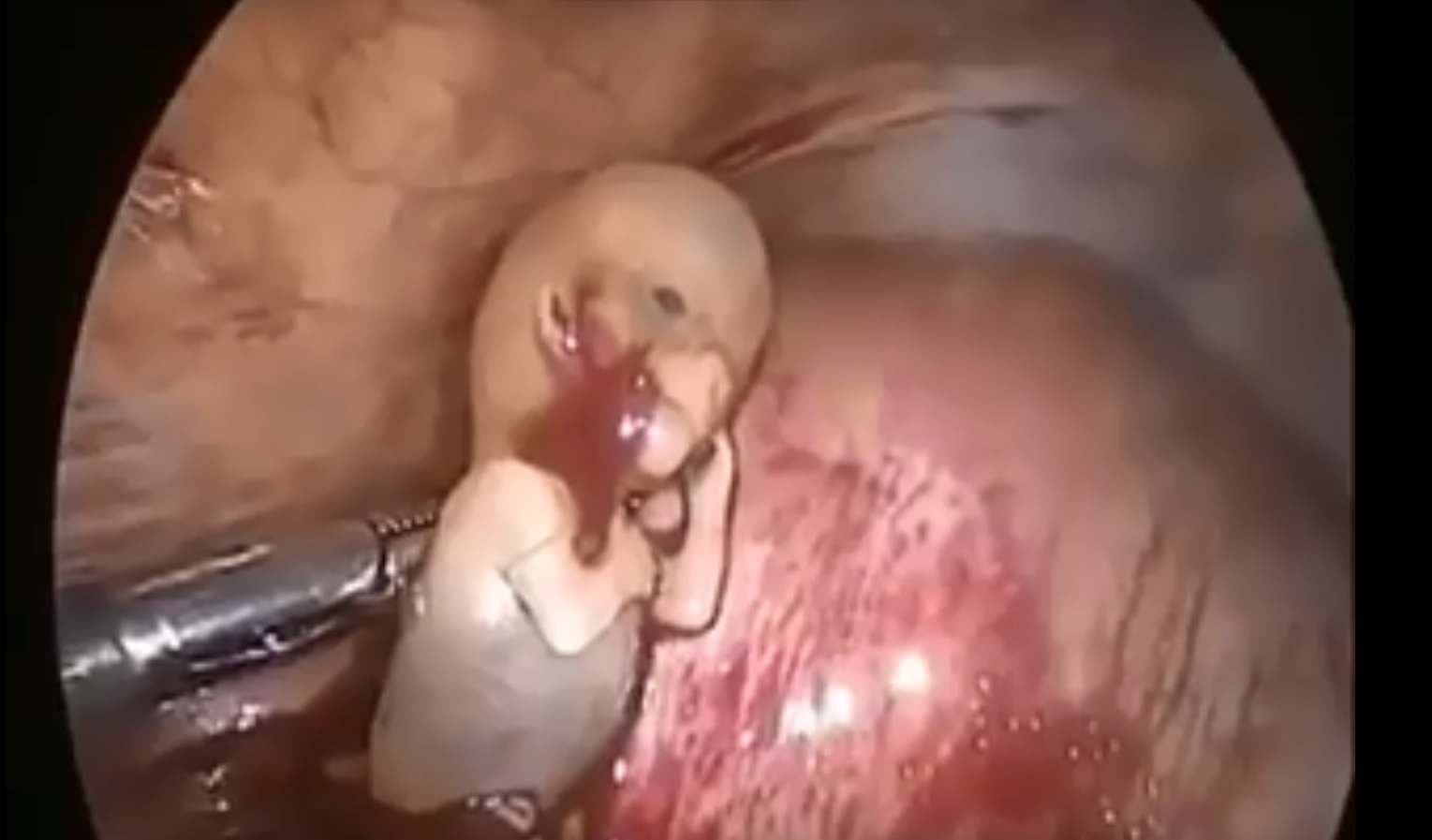
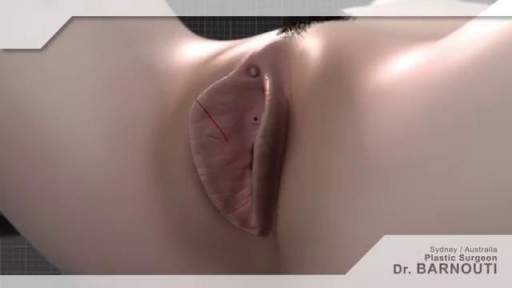
he inflatable penile prosthesis consists of two attached cylinders -- a reservoir and a pump -- which are placed surgically in the body. The two cylinders are inserted in the penis and connected by tubing to a separate reservoir of saline. The reservoir is implanted under the rectus muscles in the lower abdomen.

#tummytucksurgery #tummytuckcost #tummytuckresult #drprashantyadav #dezireclinicindia #cosmeticsurgery #plasticsurgery #weightloss #tummytuck #abdominoplasty
Tummy tuck surgery | Weight Loss
Tummy Tuck Marking before surgery
Tummy Tuck Surgery , Tummy Tuck Surgery Cost, Weight Loss with Tummy tuck surgery, tummy tuck surgery result , tummy tuck cost, Abdominoplasty
📞 Delhi - +91 8956880644 | Pune - +91 9222122122 | Bangalore- 8971224700 | Gurugram - 9272007896 | Ahmedabad - 9711162746
Subscribe to our Channel https://www.youtube.com/dezireclinic
💸Cost: call for free consultation | Zero % interest finance options
Subscribe on YouTube : https://youtube.com/dezireplas....ticsurgerycenter?sub
Subscribe on YouTube https://youtube.com/dezireclin....ic?sub_confirmation=
📸 https://www.instagram.com/drprashantdezireclinic/
🌐 http://dezireclinic.in/
Facebook: https://www.facebook.com/drprashantmch/
Twitter: https://twitter.com/drprashantmch
Email: dezireclinicindia@gmail.com
WHY choose Dezire plastic surgery center?
We are leading cosmetic surgery centre in India leading by Dr Prashant Yadav . See hundreds of various cosmetic surgery and real feedback videos. Watch live surgery to gain confidence before deciding surgery
Dr. Prashant Yadav
M.S., M.Ch. (Plastic & Cosmetic Surgery)
#plasticsurgery #cosmeticsurgery #dezireclinicindia #drprashantyadav #dezireplasticsurgerycenter

This animation shows you how a tummy tuck is performed at Boerhaave Medical Centre. Curious? Watch the video!
Boerhaave Medical Centre sets itself the goal of providing the highest quality care. Quality not just in terms of treatment, but also in terms of our staff and the before and after care given. By providing thorough information and clear advice in advance, carefully supporting our patients through the procedure and caring for them afterwards, we believe this quality is assured.
Although we are one of the largest clinics in the Netherlands and have built up many years of experience, we continuously strive to improve. After all, the Boerhaave Medical Centre intends to remain a pioneer in the healthcare sector, by working in accordance with the latest medical findings and techniques both now and in the future.
We offer the highest standard of plastic surgery in our cosmetic care department. For 365 days a year, you can also come to us for non-surgical treatments, such as injectables, permanent hair removal and gastric balloons.
We have been awarded the ZKN quality mark and are certified to ISO 9001-2008 for giving advice and carrying out plastic surgery, including after care.
Visit our website for more information: https://www.boerhaave.com/all-....treatments/upperbody
Follow us:
Facebook: https://www.facebook.com/boerhaavemc
Google+: https://plus.google.com/+BoerhaaveNl-Kliniek
Pinterest: https://nl.pinterest.com/BoerhaaveMC/
Instagram: https://www.instagram.com/BoerhaaveMC/

The examination room should be quiet, warm and well lit. After you have finished interviewing the patient, provide them with a gown (a.k.a. "Johnny") and leave the room (or draw a separating curtain) while they change. Instruct them to remove all of their clothing (except for briefs) and put on the gown so that the opening is in the rear. Occasionally, patient's will end up using them as ponchos, capes or in other creative ways. While this may make for a more attractive ensemble it will also, unfortunately, interfere with your ability to perform an examination! Prior to measuring vital signs, the patient should have had the opportunity to sit for approximately five minutes so that the values are not affected by the exertion required to walk to the exam room. All measurements are made while the patient is seated. Observation: Before diving in, take a minute or so to look at the patient in their entirety, making your observations, if possible, from an out-of-the way perch. Does the patient seem anxious, in pain, upset? What about their dress and hygiene? Remember, the exam begins as soon as you lay eyes on the patient. Temperature: This is generally obtained using an oral thermometer that provides a digital reading when the sensor is placed under the patient's tongue. As most exam rooms do not have thermometers, it is not necessary to repeat this measurement unless, of course, the recorded value seems discordant with the patient's clinical condition (e.g. they feel hot but reportedly have no fever or vice versa). Depending on the bias of a particular institution, temperature is measured in either Celcius or Farenheit, with a fever defined as greater than 38-38.5 C or 101-101.5 F. Rectal temperatures, which most closely reflect internal or core values, are approximately 1 degree F higher than those obtained orally. Respiratory Rate: Respirations are recorded as breaths per minute. They should be counted for at least 30 seconds as the total number of breaths in a 15 second period is rather small and any miscounting can result in rather large errors when multiplied by 4. Try to do this as surreptitiously as possible so that the patient does not consciously alter their rate of breathing. This can be done by observing the rise and fall of the patient's hospital gown while you appear to be taking their pulse. Normal is between 12 and 20. In general, this measurement offers no relevant information for the routine examination. However, particularly in the setting of cardio-pulmonary illness, it can be a very reliable marker of disease activity. Pulse: This can be measured at any place where there is a large artery (e.g. carotid, femoral, or simply by listening over the heart), though for the sake of convenience it is generally done by palpating the radial impulse. You may find it helpful to feel both radial arteries simultaneously, doubling the sensory input and helping to insure the accuracy of your measurements. Place the tips of your index and middle fingers just proximal to the patients wrist on the thumb side, orienting them so that they are both over the length of the vessel.

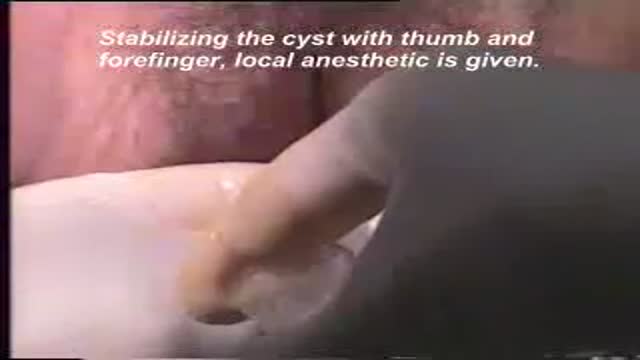
Identify the anatomy and explain the physiology of the scrotum on diagrams and sonograms.
Describe and demonstrate the protocol for sonographic scanning of the scrotum.
Identify and describe sonographic images of congenital abnormalities of the scrotum.
Identify and describe sonographic images of pathologies of the scrotum.
Identify and describe sonographic images of extratesticular disease processes.
Identify the anatomy and explain the physiology of the prostate on diagrams and sonograms.
Describe and demonstrate the protocol for transabdominal and endorectal sonographic scanning of the prostate.
Identify and describe sonographic images of benign and malignant pathologies of the prostate, including benign hyperplasia, prostatitis, carcinoma, and calculi.
Explain the technique for prostate biopsy.
Define the criteria for an ultrasound appearance of prostate tumor staging.
Explain the technique for radiation seed implantation.
Explain the Patient Privacy Rule (HIPAA) and Patient Safety Act (see reference).
Overview
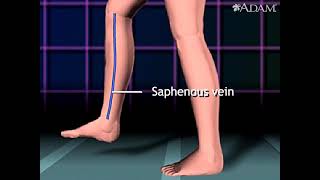
Heart bypass surgery creates a new route, called a bypass, for blood and oxygen to reach the heart.
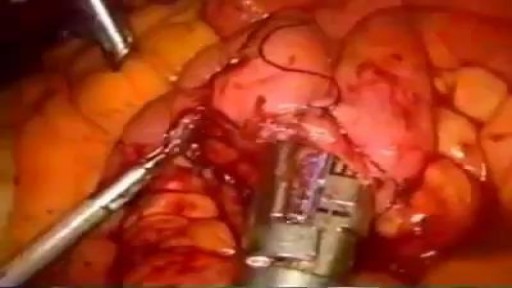
Heart bypass surgery begins with an incision in the chest, and the breastbone is cut exposing the heart. Next, a portion of the saphenous vein, which is very large, is harvested from the inside of the leg. Pieces of this large vein are used to bypass the blocked coronary arteries, which are arteries that supply blood to the heart. The venous graft is sewn to the aorta, the main artery of the body, and to the affected coronary artery, to bypass the blocked site.
The internal mammary artery from the chest may also be used to bypass a clogged artery.
Several arteries may be bypassed depending on the condition of the heart. After the graft is created, the breastbone and chest are closed.