Top videos
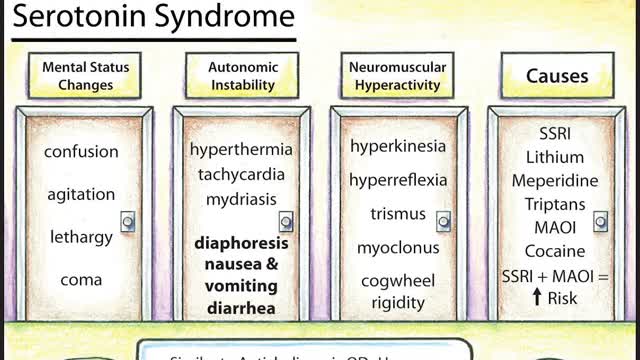
Symptoms of serotonin syndrome include a classic triad of mental status changes (eg, anxiety, delirium, confusion, restlessness), autonomic dysregulation (eg, diaphoresis, tachycardia, hypertension, hyperthermia, diarrhea, mydriasis), and neuromuscular hyperactivity (eg, hyperreflexia, tremor, rigidity, myoclonus, ocular clonus). Serotonin syndrome is clinically diagnosed and laboratory tests are used to rule out other etiologies. It usually occurs due to inadvertent interactions between drugs, therapeutic use of multiple serotonergic agents, or serotonergic medication overdose. Treatment involves discontinuation of serotonergic drugs, supportive measures, and sedation with benzodiazepines. In severe cases, a serotonin antagonist (cyproheptadine) may be used.
For strong lungs, chew 3 to 5 peppermint leaves each day. To treat congestion, add a few drops of peppermint oil to a pot of hot water and inhale the steam. You can also drink 2 cups of peppermint tea daily. To make the tea, add 1 teaspoon of dried peppermint leaves to a cup of hot water.

Intra-abdominal abscess continues to be an important and serious problem in surgical practice. Appropriate treatment is often delayed because of the obscure nature of many conditions resulting in abscess formation, which can make diagnosis and localization difficult. Associated pathophysiologic effects may become life threatening or lead to extended periods of morbidity with prolonged hospitalization. Delayed diagnosis and treatment can also lead to increased mortality; therefore, the economic impact of delaying treatment is significant.

The surgical procedure uses your own fat, so it is the most natural way to augment your buttocks. Over the last few years, the buttocks have received more press coverage than ever before. People of all ages and body types are having the Brazilian Butt Lift procedure.
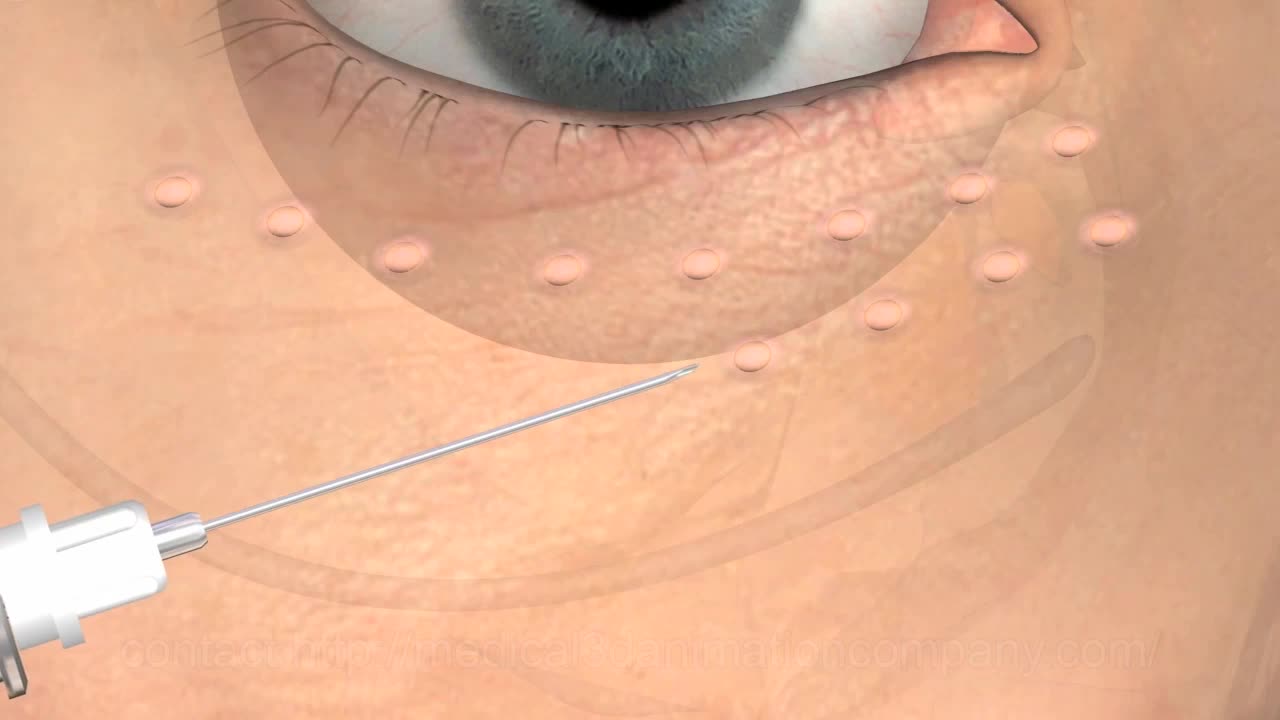
Transvenous cardiac pacing, also called endocardial pacing, is a potentially life saving intervention used primarily to correct profound bradycardia. It can be used to treat symptomatic bradycardias that do not respond to transcutaneous pacing or to drug therapy.

Physical assessment is taking an educated, systematic look at all aspects of an individual’s health status utilizing knowledge, skills and tools of health history and physical exam. To collect data- information about the client’s health, including physiological, psychological, sociocultural and spiritual aspects To establish actual and potential problems To establish the nurse-client relationship Method: The history is done first, then the physical examination focuses on finding data associated with the history. Health History- obtained through interview and record review. Physical exam- accomplished by tools and techniques ** A complete assessment is not necessarily carried out each time. A comprehensive assessment is part of a health screening examination. On admission, you will do an admission assessment (not necessarily including everything presented here) and document it on the admission form. You will do a daily shift assessment (patient systems review). And, if client has a specific problem, you may assess only that part of the body (focused). Data Collection: Information is organized into objective and subjective data: Subjective: Apparent only to person affected; includes client’s perceptions, feelings, thoughts, and expectations. It cannot be directly observed and can be discovered only asking questions. Objective: Detectable by an observer or can be tested against an acceptable standard; tangible, observable facts; includes observation of client behavior, medical records, lab and diagnostic tests, data collected by physical exam. ** To obtain data for the nursing health history, you must utilize good interview techniques and communications skills. Record accurately. DO NOT ASSUME. D. Frameworks for Health Assessment There are two main frameworks utilized in health assessment: Head to Toe- systematic collection of data starting with the head and working downward. Functional Health Assessment- Gordon’s 11 functional health patterns that address the behaviors a person uses to maintain health. PERSON is the ACC-ADN framework for assessment. It is similar to Gordon's functional health patterns.

Patient Greg Grindley communicates with host Bryant Gumbel and his wife for the first time while undergoing deep brain stimulation surgery at University Hospital's Case Medical Center in Cleveland, Ohio.
➡ Subscribe: http://bit.ly/NatGeoSubscribe
About National Geographic:
National Geographic is the world's premium destination for science, exploration, and adventure. Through their world-class scientists, photographers, journalists, and filmmakers, Nat Geo gets you closer to the stories that matter and past the edge of what's possible.
Get More National Geographic:
Official Site: http://bit.ly/NatGeoOfficialSite
Facebook: http://bit.ly/FBNatGeo
Twitter: http://bit.ly/NatGeoTwitter
Instagram: http://bit.ly/NatGeoInsta
Greg's First In-Surgery Conversation | Brain Surgery Live
https://youtu.be/zvqV_2zncNU
National Geographic
https://www.youtube.com/natgeo
Rectal bleeding can refer to any blood that passes from your anus, although rectal bleeding is usually assumed to refer to bleeding from your lower colon or rectum. Your rectum makes up the last few inches of your large intestine. Rectal bleeding may show up as blood in your stool, on the toilet paper or in the toilet bowl. Blood that results from rectal bleeding can range in color from bright red to dark maroon to a dark, tarry color.
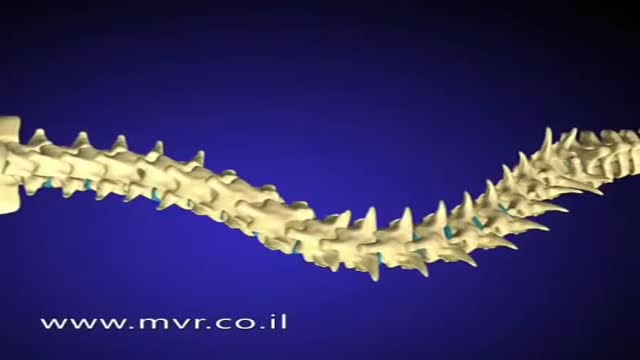
There are several approaches to scoliosis surgery, but all use modern instrumentation systems in which hooks and screws are applied to the spine to anchor long rods. The rods are then used to reduce and hold the spine while bone that is added fuses together with existing bone.