Top videos

Don't let your wrinkles reveal your age. Get rid of ageing lines with botox. Book your appointment, Call at +918939636222, +9189398 81919. For more visit - https://www.dermatologistchennai.in/anti-aging-treatment-in-nungambakkam.php

METHODS:
Previously existing methods are characterized by unpleasant scars that, despite surgeons promises, remain for life.
Incisions are:
- around the areola (Round block) leading to a flat areola, often unpleasant hypertophic skars, skin rippling.
- inverted T (around the areola, vertically down and in the fold under the breast).
- Vertical (around the areola and vertically down). Due to the extess skin, incisions often turn into inverted L or T. Rearrangement of glandular tissue and skin changes the shape of the breasts and may be different from expectations. Scars worry patients and sometimes cause disturbances in the relationship with their partner.
- No scars. The "Serdev Suture" lifting technique for breast lifting without scars (only points - needle perforations in the skin) is created by the Bulgarian cosmetic surgeon Prof. Dr. Nikolay Serdev. It is a novelty that had changed the cosmetic surgery world in the last 10-14 years for young patients. The technique is especially important in Asia and Latin America, for Asians, African-Americans, Indians, and others who form keloids and lumpy scars after operations.
The Serdev suture method can achieve lift upto and over 14 centimeters and is most suitable for the following types of breasts:
- not very heavy full breasts.
- in the presence of subpectoral implants with subsequent drooping of the breasts after childbirth and lactation.
- empty and loose breasts after childbirth and breastfeeding. In such cases this technique is combined with subpectoral implants. In sagging breasts implants should not be placed in the skin over the pectoral muscles, because thus will lead to even more drooping. Therefore, breast lift requires breast fixation to the level of the pectoral muscle (the normal position in young women), and then placement of appropriate implants under the muscle, to hold them in the appropriated position.
- in drooping breasts after subglandular augmentation (over the muscle). In such cases, patients should not wait until the skin elongation becomes visible. The implants should be removed, the capsule removed - a difficult but a necessary operation, preventing postop seromas and infection. Implants should be placed under the pectoralis muscle to wear them. Patients should orient the cosmetic surgeon at what level they want the nipples - in the middle of the implant, higher or lower.
Implants should be generally replaced - below the muscle implants should be smooth, move naturally without hurting the muscle.
Because of modern anesthetics and new methods without trauma, pain and swelling after surgery are not significant. In 3-4 days, patients can return to social life, even the next day, but it is preferable to rest for 2-3 days.
Exercises with the arms and weight lifting is prohibited for a month and a half.
Due to lack of scars, the breast lift using the Serdev sutures can be repeated to maintain the aesthetic appearence of the breasts even in advanced age.
Gigantomastia i.e. very large, very heavy and drooping breasts can not be operated in this manner, because of gravity and overskin.
Early mastopexy using Serdev sutures is recommended before too much changes in the tissues. If late, more and more complex interventions are required.
"A lot of people are opting for various breast procedures and one of the most common among them is “mastopexy”. This is the surgery that involved uplifting of sagging breasts and, in certain cases, repositioning of the nipple and areola in order to restore normality and beauty. The excess skin is removed and firmness is provided to the breasts. Though mastopexy can be done as a stand alone surgery, many people combine it with breast augmentation which involves inserting implants inside the b
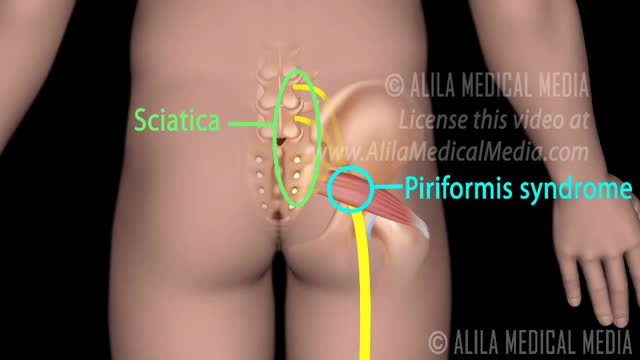
In this medical video: This 72-year-old patient was unable to resist blinking when we tapped on the glabella. This is the glabellar reflex or Myerson's sign . It is often an early sign of Parkinson's disease, but can also be seen in early dementia as well as other progressive neurologic illness. Note the left (i.e., asymmetrical) hand resting tremor.

The obstetric examination is distinct from other examinations in that you, the clinician, are trying to assess the health of two individuals – the mother and the fetus – simultaneously. From the initial history, you should be able to judge the health of the pregnancy, any risk factors that need to be addressed, and any concerns from the parents. The history is an opportunity for you to find out how much the parents know about pregnancy, labour and delivery and if they have any preferences to which these events are carried out. A carefully taken history will also direct your attention to specific signs during the examination. As such, it is important that you develop a concise and systematic method of taking the history and carrying out the examination so that you do not miss any important information. This article focuses primarily on the examination. Pregnancy is a sensitive issue, especially for the primigravida’s. Therefore, extra care is needed when you approach a pregnant woman. Always obtain expressed informed consent before examining her and have a chaperone accompany you throughout the examination. A walk-through of what you will be doing is a good way of reassuring the patient and allows the examination to go on smoothly. It is also important to let your patient know that if the examination is too painful, she can stop at any time she wants. Finally, before you begin, you should always wash your hands, especially at an OSCE station.

General Considerations Because a discussion of reproductive issues may be difficult for some women, it is important to obtain the history in a relaxed and private setting. The patient should be clothed, particularly if she is meeting the provider for the first time. Ordinarily, the patient should be interviewed alone. Exceptions may be made for children, adolescents, and mentally impaired women, or if the patient specifically requests the presence of a caretaker, friend, or family member. However, even in these circumstances, it is desirable for the patient to have some time to speak with the clinician privately. The manner of address should be formal using the title Mrs., Ms., Miss, or Dr. with the patient’s surname, unless the patient requests otherwise. In some settings, it may be appropriate for nursing staff to be involved with history taking. A nurse may be perceived as less threatening, and may be able to take the history in a less hurried manner.1 The provider can verify the history and focus on areas of concern. Alternatively, it may be helpful to ask the patient to complete a self-history form on paper or by computer prior to speaking with the provider. This allows the provider to devote time to addressing positive responses, and ensures that important questions are not missed. Hasley2 showed that responses to a computer-based questionnaire designed to update a patient’s gynecologic history were equivalent to those obtained during a personal interview. Several studies involving patients in non-gynecologic settings have shown that patients are more likely to provide sensitive information when responding to a computer-based questionnaire as opposed to a personal interview or even a paper questionnaire.3 In order to increase a patient’s level of comfort during the interview, questions should be asked in an open-ended and nonjudgmental way. Assumptions should not be made about aspects of the patient’s background such as sexual orientation. At the conclusion of the interview, patients should be asked whether there are concerns that they would like to discuss that were not addressed previously in the interview.
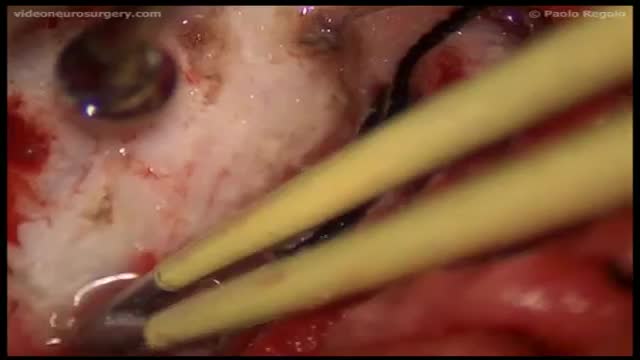
Chordoid meningioma, classified as atypical meningioma according to the World Health Organisation (WHO) classification, is a rare subtype, which represents only 0.5% of all meningiomas and is associated with a high incidence of recurrence. Multiple intracranial meningiomas are rare in non-neurofibromatosis patients. We present a female patient with both of these rare types of meningioma. The patient presented with two concurrent intracranial meningiomas, with one a meningotheliomatous subtype and the other a chordoid meningioma. Given the wide array of histological differential diagnoses in chordoid meningioma, immunohistochemistry has a significant role to play in differentiating them. Recurrence in chordoid meningioma can be generally predicted based on the extent of resection, the percentage of chordoid element, and proliferation indices.