Top videos

Alcoholic hepatitis is inflammation of the liver caused by drinking alcohol. Alcoholic hepatitis is most likely to occur in people who drink heavily over many years. However, the relationship between drinking and alcoholic hepatitis is complex. Not all heavy drinkers develop alcoholic hepatitis, and the disease can occur in people who drink only moderately. If you're diagnosed with alcoholic hepatitis, you must stop drinking alcohol. People who continue to drink alcohol face a high risk of serious liver damage and death.
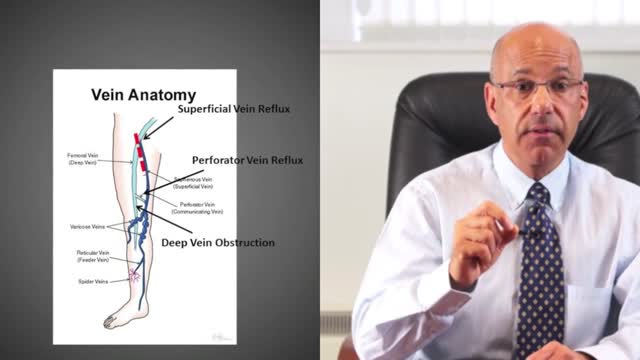
A leg ulcer is simply a break in the skin of the leg, which allows air and bacteria to get into the underlying tissue. This is usually caused by an injury, often a minor one that breaks the skin. In most people such an injury will heal up without difficulty within a week or two. However, when there is an underlying problem the skin does not heal and the area of breakdown can increase in size. This is a chronic leg ulcer.
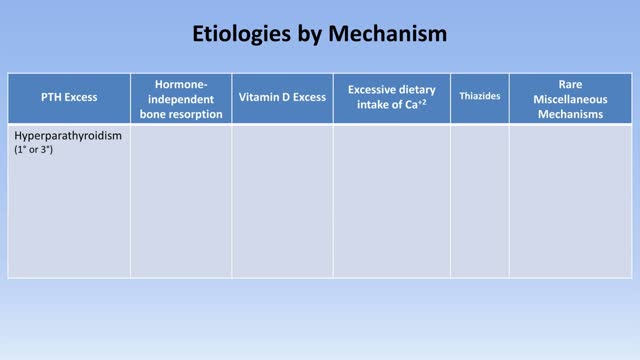
Hypercalcemia is a condition in which the calcium level in your blood is above normal. Too much calcium in your blood can weaken your bones, create kidney stones, and interfere with the way your heart and brain works. Hypercalcemia most commonly results from overactive parathyroid glands. These four tiny glands are each about the size of a grain of rice and are located on or near the thyroid gland. Other causes of hypercalcemia include cancer, certain other medical disorders, some medications, and excessive use of calcium and vitamin D supplements. Signs and symptoms of hypercalcemia may range from nonexistent to severe. Treatment depends on the underlying cause.

Are most spiders poisonous? The majority of the 3,000 spiders in the United States aren’t poisonous. Even if most spiders did bite, their fangs are too small or weak to puncture human skin. Their bites may leave itchy, red wounds that heal within a week or so. The spiders that do manage to bite through our skin and insert toxic venom can cause serious health complications. Read on to learn what spider bites look like, what spider varieties leave certain bites, and how to treat spider bites. What do spider bites look like? Identifying a spider bite is easier if you saw the spider that bit you, but it’s possible that you won’t notice the wound until hours later. Look for things like: swelling a red welt skin damage any troubling symptoms that accompany the bite Other possible symptoms that may accompany a spider bite include: itching or rash pain around the area of the bite muscle pain or cramping blister that’s red or purple in color sweating difficulty breathing headache nausea and vomiting fever chills anxiety or restlessness rashes swollen lymph glands high blood pressure Spider bites often take longer to heal than other insect bites, and they may affect skin tissues. It’s important to keep the bite clean to reduce the risk of infection. How to treat a spider bite at home In some cases, you can treat spider bites at home. For nonvenomous spider bites, follow these steps: Apply an ice pack on and off the bite for 10 minutes at a time. Elevate the area to reduce swelling. Take an antihistamine, such as diphenhydramine (Benadryl), to help with itching. Clean the area with soap and water to prevent infection. Apply antibiotic ointment to the area if blisters develop. Seek medical attention if you’re showing symptoms of a spider bite or if the symptoms don’t go away over time. Always seek medical attention if you suspect you’ve been bitten by one of the following species: brown recluse black widow hobo spider tarantula Brazilian wandering spider
Erectile dysfunction (ED) is the inability to get or keep an erection firm enough for sexual function. It’s a common sexual problem, affecting as many as 30 million men in the United States. Most cases of ED have a physical cause, such as heart disease, diabetes, and obesity. Lifestyle choices like smoking and drinking excessive amounts of alcohol can also lead to ED. But for some men, psychological issues are the root of the problem.

Hysteroscopy is a procedure that allows your doctor to look inside your uterus in order to diagnose and treat causes of abnormal bleeding. Hysteroscopy is done using a hysteroscope, a thin, lighted tube that is inserted into the vagina to examine the cervix and inside of the uterus.
Thalassemia (thal-uh-SEE-me-uh) is an inherited blood disorder characterized by less hemoglobin and fewer red blood cells in your body than normal. Several types of thalassemia exist, including alpha-thalassemia, beta-thalassemia intermedia, Cooley's anemia and Mediterranean anemia. Hemoglobin is the substance in your red blood cells that allows them to carry oxygen. The low hemoglobin and fewer red blood cells of thalassemia may cause anemia, leaving you fatigued. If you have mild thalassemia, you may not need treatment. But, if you have a more severe form of thalassemia, you may need regular blood transfusions. You can also take steps on your own to cope with fatigue, such as choosing a healthy diet and exercising regularly.

You might not notice signs or symptoms of Hashimoto's disease at first, or you may notice a swelling at the front of your throat (goiter). Hashimoto's disease typically progresses slowly over years and causes chronic thyroid damage, leading to a drop in thyroid hormone levels in your blood. The signs and symptoms are mainly those of an underactive thyroid gland (hypothyroidism). Signs and symptoms of hypothyroidism include: Fatigue and sluggishness Increased sensitivity to cold Constipation Pale, dry skin A puffy face Hoarse voice Unexplained weight gain — occurring infrequently and rarely exceeding 10 to 20 pounds, most of which is fluid Muscle aches, tenderness and stiffness, especially in your shoulders and hips Pain and stiffness in your joints and swelling in your knees or the small joints in your hands and feet Muscle weakness, especially in your lower extremities Excessive or prolonged menstrual bleeding (menorrhagia) Depression

The E.coli bacteria has claimed 14 lives and infected more than 300 hundred in the country. It has now spread to other European states.
Facing an increasing number of cases, German health authorities warned people to avoid eating raw cucumber, tomatoes and lettuce.
Reinhard Burger, President of Robert Koch Institute, said, "As for the present situation there is no reason to give the all-clear yet and it is possible the original source of the infection is still active and could lead to further infections."
The first cases of the EHEC outbreak were noticed in Northern Germany, but infections are now spreading across the country.
Cases haves spiked compared to other years, and are still rising.
Daniel Bahr, German Health Minister, said, "The result is that we unfortunately still have to prepare for a rising number of cases. Exercising caution is still recommended and we ask our citizens to be particularly careful. "
But, the German government says it's working around the clock to stop the outbreak and clarify how it arose.
Ilse Aigner, German Agriculture Minister, said, "Together, we face a big challenge to piece together hundreds or thousands of mosaic pieces from Germany and abroad into an overall picture that gives us a clear answer on how this terrible infection arose. "
In the meantime, experts are advising not to eat pre-packaged or prepared salad, which may contain the bacteria.