Top videos
In this medical video: This 72-year-old patient was unable to resist blinking when we tapped on the glabella. This is the glabellar reflex or Myerson's sign . It is often an early sign of Parkinson's disease, but can also be seen in early dementia as well as other progressive neurologic illness. Note the left (i.e., asymmetrical) hand resting tremor.
Thoracic outlet syndrome affects the space between the collarbone and first rib (thoracic outlet). Common causes include trauma, repetitive injuries, pregnancy, and anatomical defects, such as having an extra rib. Symptoms include pain in the shoulders and neck and numbness, weakness, and coldness in the fingers. Treatment involves physical therapy and pain relief. In rare cases, surgery may be needed to relieve the compression.
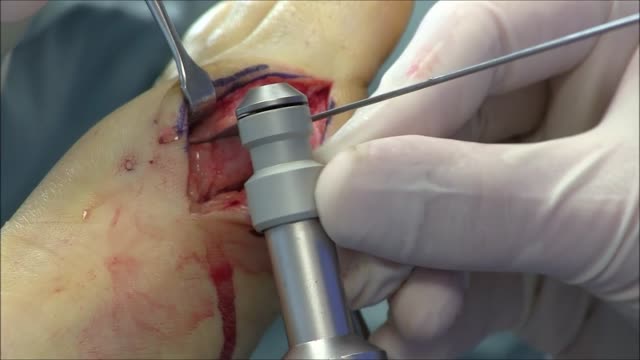
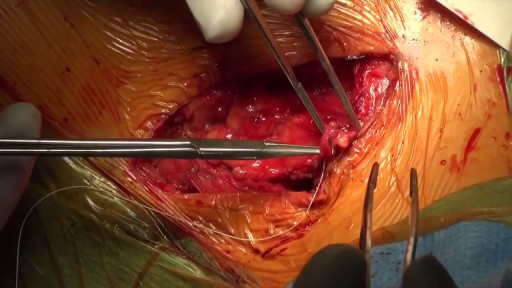
Bunions can be very painful. ... Bunion removal is a surgical procedure that corrects a deformed area of the foot near the big toe. Bunion removal is sometimes called a bunionectomy, bunion surgery, or hallux valgus correction. Hallux valgus is a Latin phrase that means “foot deformity
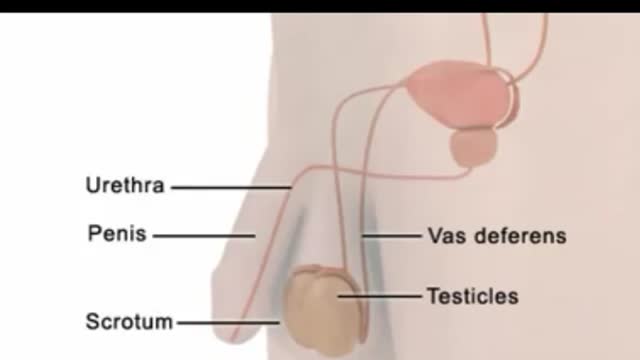
An egg cannot be fertilized when there are no sperm in the semen. The testicles continue to produce sperm, but the sperm are reabsorbed by the body. (This also happens to sperm that are not ejaculated after a while, regardless of whether you have had a vasectomy.) Sperm are made in the testicles. They pass through two tubes called the vasa deferentia to other glands and mix with seminal fluids to form semen. Vasectomy blocks each vas deferens and keeps sperm out of the seminal fluid. The sperm are absorbed by the body instead of being ejaculated.
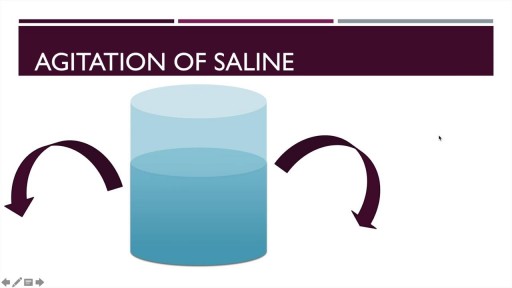
A detailed description of the Hepato-pulmonary syndrome including its definition, pathophysiology, diagnosis and treatment. The pathophysiology includes nitric oxide in the pulmonary vasculature which results in intrapulmonary vasodilatation. This causes the classical and unique symptom of platypnea and orthodeoxia.

A pneumothorax is usually caused by an injury to the chest, such as a broken rib or puncture wound. It may also occur suddenly without an injury. A pneumothorax can result from damage to the lungs caused by conditions such as chronic obstructive pulmonary disease (COPD), asthma, cystic fibrosis, and pneumonia.

General Considerations Because a discussion of reproductive issues may be difficult for some women, it is important to obtain the history in a relaxed and private setting. The patient should be clothed, particularly if she is meeting the provider for the first time. Ordinarily, the patient should be interviewed alone. Exceptions may be made for children, adolescents, and mentally impaired women, or if the patient specifically requests the presence of a caretaker, friend, or family member. However, even in these circumstances, it is desirable for the patient to have some time to speak with the clinician privately. The manner of address should be formal using the title Mrs., Ms., Miss, or Dr. with the patient’s surname, unless the patient requests otherwise. In some settings, it may be appropriate for nursing staff to be involved with history taking. A nurse may be perceived as less threatening, and may be able to take the history in a less hurried manner.1 The provider can verify the history and focus on areas of concern. Alternatively, it may be helpful to ask the patient to complete a self-history form on paper or by computer prior to speaking with the provider. This allows the provider to devote time to addressing positive responses, and ensures that important questions are not missed. Hasley2 showed that responses to a computer-based questionnaire designed to update a patient’s gynecologic history were equivalent to those obtained during a personal interview. Several studies involving patients in non-gynecologic settings have shown that patients are more likely to provide sensitive information when responding to a computer-based questionnaire as opposed to a personal interview or even a paper questionnaire.3 In order to increase a patient’s level of comfort during the interview, questions should be asked in an open-ended and nonjudgmental way. Assumptions should not be made about aspects of the patient’s background such as sexual orientation. At the conclusion of the interview, patients should be asked whether there are concerns that they would like to discuss that were not addressed previously in the interview.

The E.coli bacteria has claimed 14 lives and infected more than 300 hundred in the country. It has now spread to other European states.
Facing an increasing number of cases, German health authorities warned people to avoid eating raw cucumber, tomatoes and lettuce.
Reinhard Burger, President of Robert Koch Institute, said, "As for the present situation there is no reason to give the all-clear yet and it is possible the original source of the infection is still active and could lead to further infections."
The first cases of the EHEC outbreak were noticed in Northern Germany, but infections are now spreading across the country.
Cases haves spiked compared to other years, and are still rising.
Daniel Bahr, German Health Minister, said, "The result is that we unfortunately still have to prepare for a rising number of cases. Exercising caution is still recommended and we ask our citizens to be particularly careful. "
But, the German government says it's working around the clock to stop the outbreak and clarify how it arose.
Ilse Aigner, German Agriculture Minister, said, "Together, we face a big challenge to piece together hundreds or thousands of mosaic pieces from Germany and abroad into an overall picture that gives us a clear answer on how this terrible infection arose. "
In the meantime, experts are advising not to eat pre-packaged or prepared salad, which may contain the bacteria.

Will you still love me if I have herpes? About 1 in 6 Americans between the ages of 14 and 49 is infected with herpes simplex virus type 2, according to a health survey released by the Centers for Disease Control and Prevention. If you’re living with herpes, HSV, HPV or other STDs, you're recommended to check out the largest STD support site STDdatings.