Top videos
Caesarean section is the most common way to deliver a breech baby in the USA, Australia, and Great Britain. Like any major surgery, it involves risks. Maternal mortality is increased by a Caesarean section, but still remains a rare complication in the First World. Third World statistics are dramatically different, and mortality is increased significantly. There is remote risk of injury to the mother’s internal organs, injury to the baby, and severe hemorrhage requiring hysterectomy with resultant infertility. More commonly seen are problems with noncatastrophic bleeding, postoperative infection and wound healing problems. It should be added that the increase in maternal mortality rates could be slightly skewed due to the fact that Caesarean sections are often used during high-risk pregnancies and/or when mortality is already a strong possibility.
One large study has confirmed that elective cesarean section has lower risk to the fetus and a slightly increased risk to the mother, than planned vaginal delivery of the breech however elements of the methodology used have undergone some criticism.
The same birth injuries that can occur in vaginal breech birth may rarely occur in Caesarean breech delivery. A Caesarean breech delivery is still a breech delivery. However the soft tissues of the uterus and abdominal wall are more forgiving of breech delivery than the hard bony ring of the pelvis. If a Caesarean is scheduled in advance (rather than waiting for the onset of labor) there is a risk of accidentally delivering the baby too early, so that the baby might have complications of prematurity. The mother’s subsequent pregnancies will be riskier than they would be after a vaginal birth (uterine rupture). The presence of a uterine scar will be a risk factor for any subsequent pregnancies.
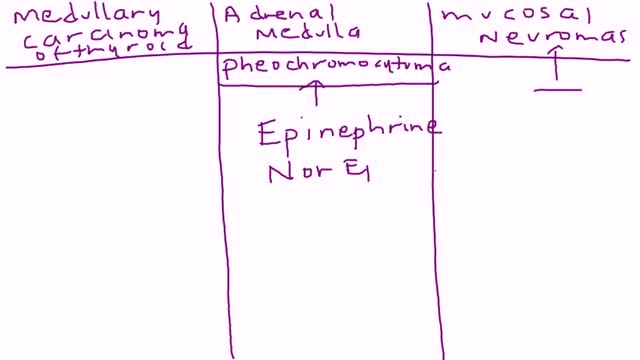
Multiple endocrine neoplasia type 2 (MEN2) is a hereditary condition associated with three primary types of tumors: medullary thyroid cancer, parathyroid tumors, and pheochromocytoma. MEN2 is classified into three subtypes based on clinical features. MEN2A, which affects 60% to 90% of MEN2 families Medullary thyroid cancer: 98% to 100% with MEN2A are affected Pheochromocytoma, a typically benign (noncancerous) tumor of the adrenal glands: 50% with MEN2A affected Parathyroid adenoma (benign tumor) or hyperplasia, meaning increased size, of the parathyroid gland: 5% to 10% with MEN2A affected MEN2B, which affects 5% of MEN2 families Medullary thyroid cancer: 98% to 100% with MEN2B affected Pheochromocytoma: 50% with MEN2B affected Mucosal neuromas, which is a benign tumor of nerve tissue on the tongue, lips and throughout the gastrointestinal tract: 95% to 98% affected Digestive problems caused by disordered nerves in the gastrointestinal tract: 75% to 90% affected Muscle, joint, and spinal problems: 95% affected Typical facial features, including swollen lips and thick eyelids: 75% to 90% affected Familial medullary thyroid cancer (FMTC), which affects 5% to 35% of MEN2 families Medullary thyroid carcinoma only Sources: Gagel RF, Marx SJ. “Multiple endocrine neoplasia.” Williams Textbook of Endocrinology, Chapter 40, 11th ed., Philadelphia, 2008, and Eng C, Clayton D, et al. Grubbs EG, Gagel RF. My, How Things Have Changed in Multiple Endocrine Neoplasia Type 2A! J Clin Endocrinol Metab 100(7):2532-5, 7/2015. PMID: 26151398. What causes MEN2? MEN2 is a genetic condition. This means that the cancer risk and other features of MEN2 can be passed from generation to generation in a family. The gene associated with MEN2 is called RET. A mutation (alteration) in the RET gene gives a person an increased risk of developing medullary thyroid cancer and other tumors associated with MEN2.
http://tmj-pain-relief.good-info.co What Is Tmj, Grinding Teeth While Sleeping, Tmj Disorder Treatment, Tmj Help, Tmj Night Guard. What is TMJ? The temporomandibular joint is the hinge joint of the jaw that connects the lower jaw (mandible) to the temporal bone of the skull. This joint is an articular disc composed of fibrocartilagenous tissue. It comprises, all in all, of six parts: mandibular condyles, articular surface of the temporal bone, capsule, articular disc, ligaments and lateral pterygoid. The TM Joint facilitates movement of the jaws, thereby allowing essential functions like talking, eating and swallowing. Needless to say, the slightest afflictions caused to this joint, disrupt a great deal of its basic functions. The most common affliction that occurs is the TMJ Disorder. So, what is TMJ Disorder? The TMJ Disorder is a term used to describe an acute inflammation of the TM Joint. It is categorized in three ways: 1.By myofascial pain: The fascia is the tissue that connects the different parts of your body. Fascia around the muscles is called myofascial. Thus, any injury to the myofascial, will automatically adversely affect the muscles. The most common TMJ disorder is associated with myofascial pain in the jaw muscles and neck. 2.By internal injury: Any dislocation, injury, or indeed, any derangement in the joint results in TMJ disorder.

A parasitic twin (also known as an asymmetrical or unequal conjoined twin) is the result of the processes that produce vanishing twins and conjoined twins, and may represent a continuum between the two. Parasitic twins occur when a twin embryo begins developing in utero, but the pair does not fully separate, and one embryo maintains dominant development at the expense of the other. Unlike conjoined twins, one ceases development during gestation and is vestigial to a mostly fully-formed, otherwise healthy individual twin. The undeveloped twin is defined as parasitic, rather than conjoined, because it is incompletely formed or wholly dependent on the body functions of the complete fetus. The independent twin is called the autosite.
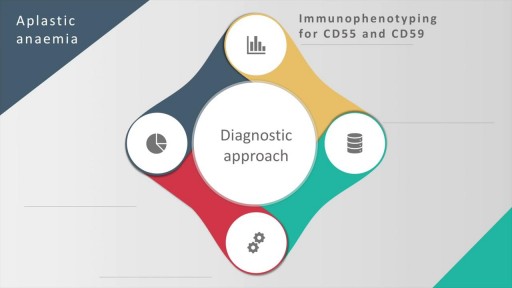
Aplastic anemia is a hematopoietic disorder caused due to T lymphocyte mediated destruction of stem cells resulting in pancytopenia with a cellular bone marrow and normal cell cytogenetics. The causes of aplastic anaemia may be inherited or acquired. The causes and the diagnostic approach, along with spectrum of severity of this disorder is discussed in this presentation. A detailed discussion of the management options, along with pharmacological therapy and supportive therapy in these cases is also discussed. The treatment options include, in addition to a stem cell transplant, anti-thymocyte globulin, cyclosporine, methyprednisolone and eltrombopag (for patients who have failed treatment on combined modality therapy with ATG and cyclosporine)
Pharyngitis is caused by swelling in the back of the throat (pharynx) between the tonsils and the voice box (larynx). Most sore throats are caused by colds, the flu, coxsackie virus or mono (mononucleosis). Bacteria that can cause pharyngitis in some cases: Strep throat is caused by group A streptococcus.
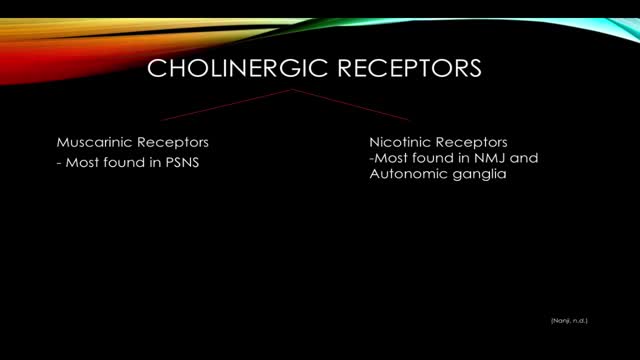
Organophosphate poisoning results from exposure to organophosphates (OPs), which cause the inhibition of acetylcholinesterase (AChE), leading to the accumulation of acetylcholine (ACh) in the body. Organophosphate poisoning most commonly results from exposure to insecticides or nerve agents.