Top videos
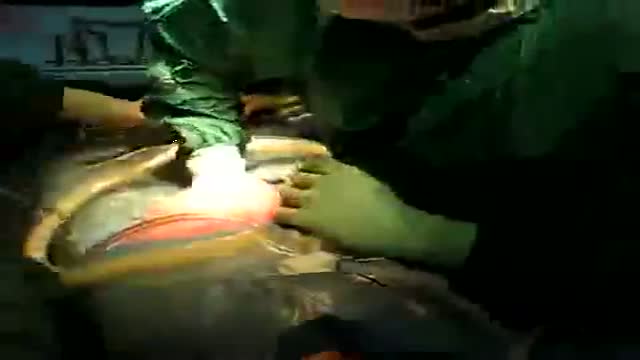
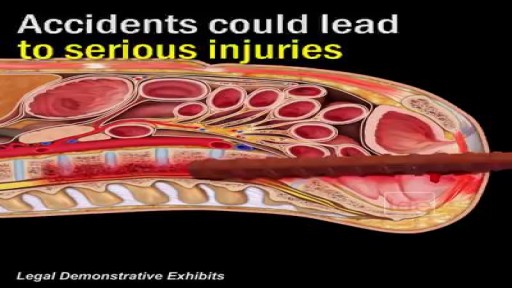
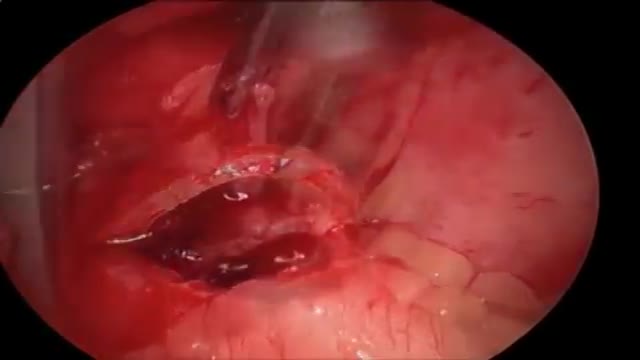
Caesarean section is the most common way to deliver a breech baby in the USA, Australia, and Great Britain. Like any major surgery, it involves risks. Maternal mortality is increased by a Caesarean section, but still remains a rare complication in the First World. Third World statistics are dramatically different, and mortality is increased significantly. There is remote risk of injury to the mother’s internal organs, injury to the baby, and severe hemorrhage requiring hysterectomy with resultant infertility. More commonly seen are problems with noncatastrophic bleeding, postoperative infection and wound healing problems. It should be added that the increase in maternal mortality rates could be slightly skewed due to the fact that Caesarean sections are often used during high-risk pregnancies and/or when mortality is already a strong possibility.
One large study has confirmed that elective cesarean section has lower risk to the fetus and a slightly increased risk to the mother, than planned vaginal delivery of the breech however elements of the methodology used have undergone some criticism.
The same birth injuries that can occur in vaginal breech birth may rarely occur in Caesarean breech delivery. A Caesarean breech delivery is still a breech delivery. However the soft tissues of the uterus and abdominal wall are more forgiving of breech delivery than the hard bony ring of the pelvis. If a Caesarean is scheduled in advance (rather than waiting for the onset of labor) there is a risk of accidentally delivering the baby too early, so that the baby might have complications of prematurity. The mother’s subsequent pregnancies will be riskier than they would be after a vaginal birth (uterine rupture). The presence of a uterine scar will be a risk factor for any subsequent pregnancies.
Johns Hopkins Children’s Center Surgeon-in-Chief David Hackam provides information about general pediatric surgery and when it is time to see a general pediatric surgeon. #PediatricSurgery #JohnsHopkins
For more information on general pediatric surgery at Johns Hopkins Children's Center, visit https://www.hopkinsmedicine.or....g/johns-hopkins-chil
FAQ's
0:02 What is a general pediatric surgeon?
0:31 When is it time to see a pediatric surgeon?
1:02 What are some of the most common surgical problems seen by general pediatric surgeons?
1:43 Describe research being done in the field.
2:15 Why choose Johns Hopkins Children's Center for general pediatric surgery?
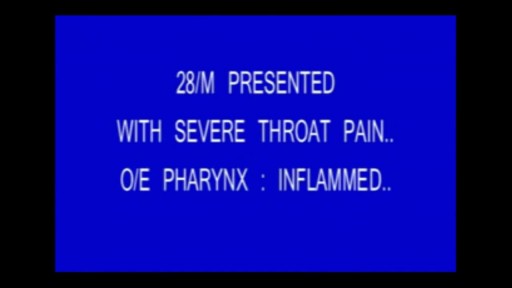
Pharyngitis is caused by swelling in the back of the throat (pharynx) between the tonsils and the voice box (larynx). Most sore throats are caused by colds, the flu, coxsackie virus or mono (mononucleosis). Bacteria that can cause pharyngitis in some cases: Strep throat is caused by group A streptococcus.
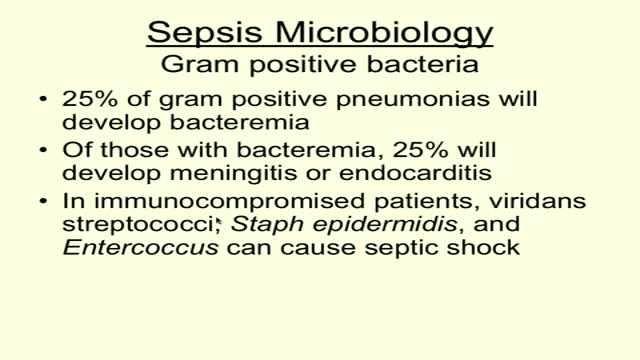
Sepsis is a potentially life-threatening complication of an infection. Sepsis occurs when chemicals released into the bloodstream to fight the infection trigger inflammatory responses throughout the body. This inflammation can trigger a cascade of changes that can damage multiple organ systems, causing them to fail. If sepsis progresses to septic shock, blood pressure drops dramatically, which may lead to death. Anyone can develop sepsis, but it's most common and most dangerous in older adults or those with weakened immune systems. Early treatment of sepsis, usually with antibiotics and large amounts of intravenous fluids, improves chances for survival. Symptoms & causes Symptoms Many doctors view sepsis as a three-stage syndrome, starting with sepsis and progressing through severe sepsis to septic shock. The goal is to treat sepsis during its early stage, before it becomes more dangerous. Sepsis To be diagnosed with sepsis, you must exhibit at least two of the following symptoms, plus a probable or confirmed infection: Body temperature above 101 F (38.3 C) or below 96.8 F (36 C) Heart rate higher than 90 beats a minute Respiratory rate higher than 20 breaths a minute Severe sepsis Your diagnosis will be upgraded to severe sepsis if you also exhibit at least one of the following signs and symptoms, which indicate an organ may be failing: Significantly decreased urine output Abrupt change in mental status Decrease in platelet count Difficulty breathing Abnormal heart pumping function Abdominal pain Septic shock To be diagnosed with septic shock, you must have the signs and symptoms of severe sepsis — plus extremely low blood pressure that doesn't adequately respond to simple fluid replacement. When to see a doctor Most often sepsis occurs in people who are hospitalized. People in the intensive care unit are especially vulnerable to developing infections, which can then lead to sepsis. If you get an infection or if you develop signs and symptoms of sepsis after surgery, hospitalization or an infection, seek medical care immediately. Causes While any type of infection — bacterial, viral or fungal — can lead to sepsis, the most likely varieties include: Pneumonia Abdominal infection Kidney infection Bloodstream infection (bacteremia) The incidence of sepsis appears to be increasing in the United States. The causes of this increase may include: Aging population. Americans are living longer, which is swelling the ranks of the highest risk age group — people older than 65. Drug-resistant bacteria. Many types of bacteria can resist the effects of antibiotics that once killed them. These antibiotic-resistant bacteria are often the root cause of the infections that trigger sepsis. Weakened immune systems. More Americans are living with weakened immune systems, caused by HIV, cancer treatments or transplant drugs. Risk factors Sepsis is more common and more dangerous if you: Are very young or very old Have a compromised immune system Are already very sick, often in a hospital's intensive care unit Have wounds or injuries, such as burns Have invasive devices, such as intravenous catheters or breathing tubes Complications Sepsis ranges from less to more severe. As sepsis worsens, blood flow to vital organs, such as your brain, heart and kidneys, becomes impaired. Sepsis can also cause blood clots to form in your organs and in your arms, legs, fingers and toes — leading to varying degrees of organ failure and tissue death (gangrene). Most people recover from mild sepsis, but the mortality rate for septic shock is nearly 50 percent. Also, an episode of severe sepsis may place you at higher risk of future infections.

A parasitic twin (also known as an asymmetrical or unequal conjoined twin) is the result of the processes that produce vanishing twins and conjoined twins, and may represent a continuum between the two. Parasitic twins occur when a twin embryo begins developing in utero, but the pair does not fully separate, and one embryo maintains dominant development at the expense of the other. Unlike conjoined twins, one ceases development during gestation and is vestigial to a mostly fully-formed, otherwise healthy individual twin. The undeveloped twin is defined as parasitic, rather than conjoined, because it is incompletely formed or wholly dependent on the body functions of the complete fetus. The independent twin is called the autosite.

http://control-blood-sugar.good-info.co Low Blood Sugar, Signs Of Low Blood Sugar, Low Iron In Blood, Normal Glucose Levels In Blood Are You Suffering From High Or Uncontrollable Blood Sugar? Because This May Be The Solution. If you’re one of the 387 million people in the world trying to win the battle against uncontrollable blood sugar or even diabetes. Then you’re in the right place, as believe it or not, these conditions can be completely reversed from the comfort of your own home in just 3 short weeks. Are you. Tired of poking your skin with expensive needles everyday? Tired of dealing with the constant lethargy and lack of energy that’s associated with your uncontrollable blood sugar? Tired of living your life with stubborn body fat on your waist, legs,and thighs? Tired of being embarrassed to go to the beach or even taking your shirt off in front of your kids? Tired of waking up with a headache in a soaked bed from sweating so much at night? If you are sick and tired of these all of these conditions and more, then I am happy to tell you that all these conditions of your uncontrollable blood sugar can be completely thrown away for good! click here. http://control-blood-sugar.good-info.co

This follow-along routine features stretching and strengthening exercises for before and after knee replacement surgery. Daljit, who is awaiting knee surgery, joins physiotherapist Milly Abdullah to demonstrate the exercises.
This video is part of the Surgery Toolkit, a series designed for people living with arthritis who are awaiting or recovering from joint replacement surgery. Staying active is important if you’re waiting for or recovering from surgery. Being fitter and stronger can improve the success of the operation and lead to a faster recovery time.
In the Surgery Toolkit you’ll also find tailor-made, follow-along exercise routines for hip and shoulder replacement, as well as full body workouts to help you maintain overall fitness. The series also includes advice films, personal stories and top tips on staying active before and after surgery from those living with arthritis who have been through joint replacement surgery.
This series is part of Let’s Move, a programme for people with arthritis who want more movement in their lives. Sign up today to the free newsletter to receive all the latest content to help you to get active in a way that works for you: https://action.versusarthritis.....org/page/120448/dat

This video shows how to perform the McMurray test, one of the most commonly used clinical assessment tools to assess for meniscal injuries in the knee.
This video clip is part of the FIFA Diploma in Football Medicine and the FIFA Medical Network. To enrol or to find our more click on the following link http://www.fifamedicalnetwork.com
The Diploma is a free online course designed to help clinicians learn how to diagnose and manage common football-related injuries and illnesses. There are a total of 42 modules created by football medicine experts. Visit a single page, complete individual modules or finish the entire course.
The network provides the opportunity for clinicians around the world to meet and share ideas relating to football medicine. Ask about an interesting case, debate current practice and discuss treatment strategies. Create a profile and log on to interact with other health professionals from around the globe.
This is not medical advice. The content is intended as educational content for health care professionals and students. If you are a patient, seek care of a health care professional.