Top videos
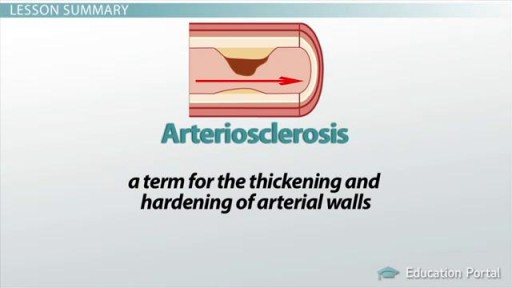
Arteriosclerosis occurs when the blood vessels that carry oxygen and nutrients from your heart to the rest of your body (arteries) become thick and stiff — sometimes restricting blood flow to your organs and tissues. Healthy arteries are flexible and elastic, but over time, the walls in your arteries can harden, a condition commonly called hardening of the arteries. Atherosclerosis is a specific type of arteriosclerosis, but the terms are sometimes used interchangeably. Atherosclerosis refers to the buildup of fats, cholesterol and other substances in and on your artery walls (plaques), which can restrict blood flow. These plaques can burst, triggering a blood clot. Although atherosclerosis is often considered a heart problem, it can affect arteries anywhere in your body. Atherosclerosis may be preventable and is treatable.
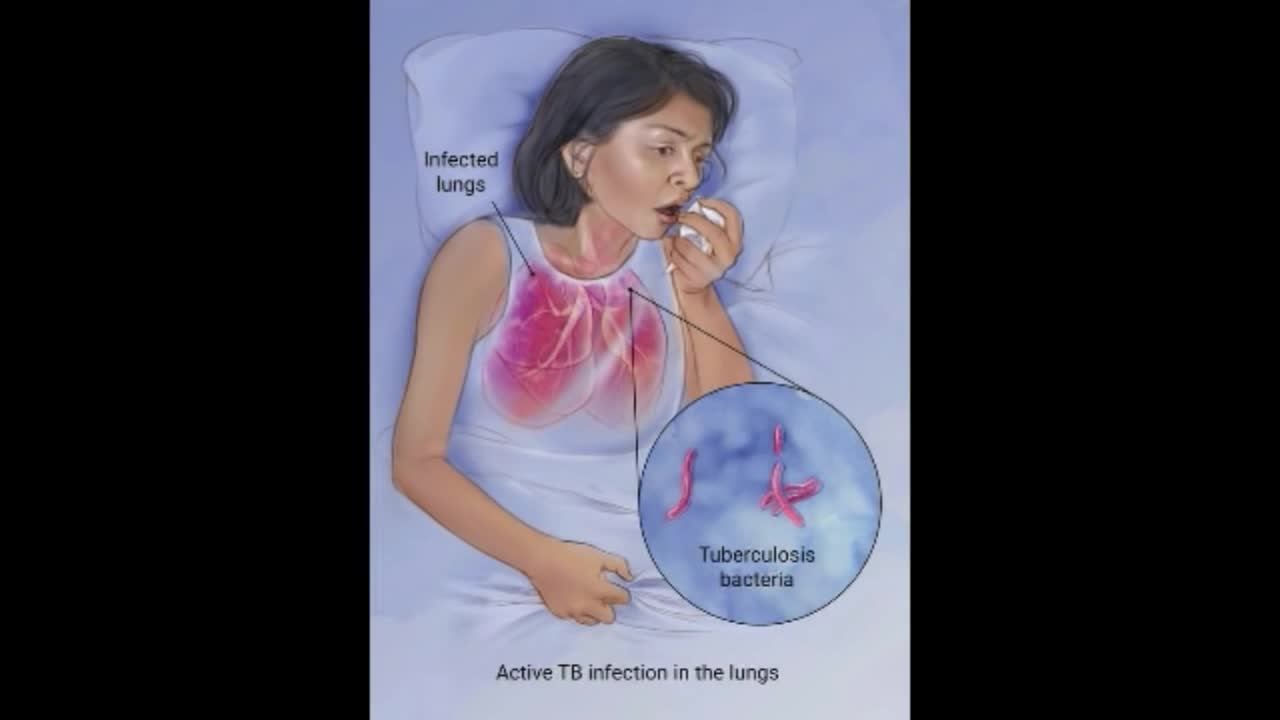
Although your body may harbor the bacteria that cause tuberculosis, your immune system usually can prevent you from becoming sick. For this reason, doctors make a distinction between: Latent TB. In this condition, you have a TB infection, but the bacteria remain in your body in an inactive state and cause no symptoms. Latent TB, also called inactive TB or TB infection, isn't contagious. It can turn into active TB, so treatment is important for the person with latent TB and to help control the spread of TB. An estimated 2 billion people have latent TB. Active TB. This condition makes you sick and can spread to others. It can occur in the first few weeks after infection with the TB bacteria, or it might occur years later. Signs and symptoms of active TB include: Coughing that lasts three or more weeks Coughing up blood Chest pain, or pain with breathing or coughing Unintentional weight loss Fatigue Fever Night sweats
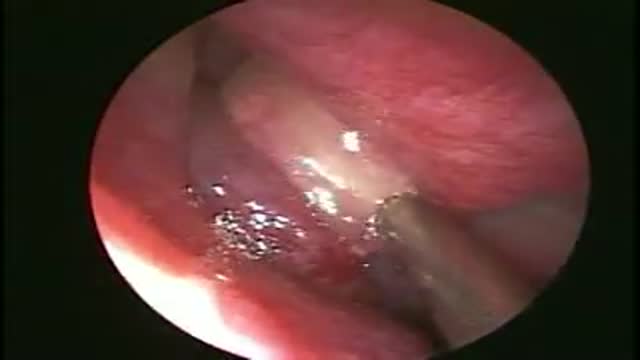
Nasal polyps are soft, painless, noncancerous growths on the lining of your nasal passages or sinuses. They hang down like teardrops or grapes. They result from chronic inflammation due to asthma, recurring infection, allergies, drug sensitivity or certain immune disorders. Nasal polyps are polypoidal masses arising mainly from the mucous membranes of the nose and paranasal sinuses. They are overgrowths of the mucosa that frequently accompany allergic rhinitis, and are freely movable and nontender.

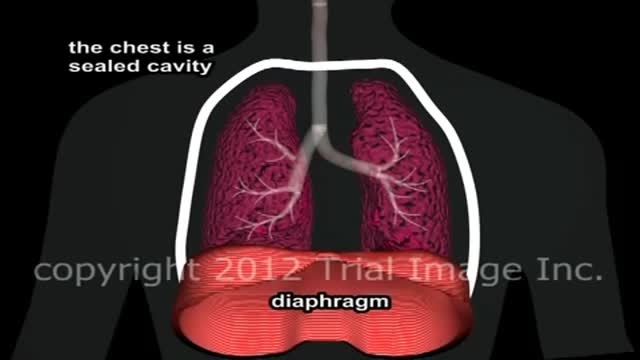
This video: Patent ductus arteriosus (PDA) is a persistent opening between two major blood vessels leading from the heart. The opening, called the ductus arteriosus, is a normal part of a baby's circulatory system before birth that usually closes shortly after birth. If it remains open, however, it's called a patent ductus arteriosus. A small patent ductus arteriosus often doesn't cause problems and might never need treatment. However, a large patent ductus arteriosus left untreated can allow poorly oxygenated blood to flow in the wrong direction, weakening the heart muscle and causing heart failure and other complications. Treatment options for a patent ductus arteriosus include monitoring, medications and closure by cardiac catheterization or surgery.
Aplastic anemia is a hematopoietic disorder caused due to T lymphocyte mediated destruction of stem cells resulting in pancytopenia with a cellular bone marrow and normal cell cytogenetics. The causes of aplastic anaemia may be inherited or acquired. The causes and the diagnostic approach, along with spectrum of severity of this disorder is discussed in this presentation. A detailed discussion of the management options, along with pharmacological therapy and supportive therapy in these cases is also discussed. The treatment options include, in addition to a stem cell transplant, anti-thymocyte globulin, cyclosporine, methyprednisolone and eltrombopag (for patients who have failed treatment on combined modality therapy with ATG and cyclosporine)
Johns Hopkins Children’s Center Surgeon-in-Chief David Hackam provides information about general pediatric surgery and when it is time to see a general pediatric surgeon. #PediatricSurgery #JohnsHopkins
For more information on general pediatric surgery at Johns Hopkins Children's Center, visit https://www.hopkinsmedicine.or....g/johns-hopkins-chil
FAQ's
0:02 What is a general pediatric surgeon?
0:31 When is it time to see a pediatric surgeon?
1:02 What are some of the most common surgical problems seen by general pediatric surgeons?
1:43 Describe research being done in the field.
2:15 Why choose Johns Hopkins Children's Center for general pediatric surgery?

What Is It? Your wisdom teeth (third molars) usually start to erupt (enter your mouth) during the late teen years. Sometimes, there's not enough room for them. They may come into your mouth partially or not at all. Partial eruption of a wisdom tooth can create a flap of gum tissue next to the tooth. The flap can trap bits of food and debris. It can turn into a hotbed for bacteria. It's called pericoronitis if the tissue around the tooth becomes inflamed. Pericoronitis also can occur around a wisdom tooth that is still completely under the gums. Symptoms Symptoms include: Painful, swollen gum tissue in the area of the affected tooth. It can be difficult to bite down comfortably without catching the swollen tissue between your teeth. A bad smell or taste in the mouth Discharge of pus from the gum near the tooth More serious symptoms include: Swollen lymph nodes under your chin (the submandibular nodes) Muscle spasms in the jaw Swelling on the affected side of the face Diagnosis Usually, someone with pericoronitis goes to the dentist, complaining of pain in the area of the back tooth. Pericoronitis is diagnosed during the clinical exam. Your dentist will see inflamed gum tissue in the area of the unerupted or partly erupted wisdom tooth. The gums may be red, swollen or draining fluid or pus. Expected Duration Pericoronitis can be managed with antibiotics and warm salt water rinses. It goes away in about one week. However, it can return. This is likely to happen if the tooth does not completely enter the mouth and food and bacteria keep building up under the gum. Prevention You can help to prevent pericoronitis by brushing any erupting wisdom tooth and flossing around it. This will help make sure that food and bacteria do not build up under the gums. However, sometimes these steps do not work. If pericoronitis returns, you may need to have the flap of gum tissue removed. In some cases, the flap of tissue grows back and the wisdom tooth will need to be extracted. Treatment Pericoronitis can be tricky to treat. That's because the flap of gum tissue won't go away until the wisdom tooth emerges naturally, the tissue is removed or the tooth is removed. Your dentist will clean the area thoroughly by rinsing under the flap with water to remove bits of food and pus. Your dentist also may need to remove damaged tissue. If the area is infected, you'll most likely be given antibiotics. Your dentist will explain how to keep the area clean, which is the best way to prevent the problem from returning. This usually involves brushing and flossing daily and rinsing your mouth with water several times a day. These steps will help to prevent food from getting stuck under the gum flap. In some cases, your dentist may suggest removing the erupting tooth. Or the dentist may want to remove the tooth above it, which bites down on the gum below. If your dentist thinks the tooth may erupt fully into the mouth without problems, he or she may leave it alone. However, if pericoronitis comes back, the tooth may be extracted. Pericoronitis that causes symptoms should be treated as soon as possible. If it is not, the infection can spread to other areas of your mouth. The most severe cases are treated in a hospital. They sometimes require intravenous antibiotics and surgery. When To Call a Professional If you have symptoms of pericoronitis, make an appointment to see your dentist. If your wisdom teeth are coming in, visit your dentist at least twice a year for regular checkups. During those visits, the dentist can check on the progress of your wisdom teeth. Prognosis Pericoronitis does not cause any long-term effects. If the affected tooth is removed or erupts fully into the mouth, the condition cannot return.
Pulmonary edema Email this page to a friend Email this page to a friend Facebook Twitter Google+ Pulmonary edema is an abnormal buildup of fluid in the lungs. This buildup of fluid leads to shortness of breath. Causes Pulmonary edema is often caused by congestive heart failure. When the heart is not able to pump efficiently, blood can back up into the veins that take blood through the lungs. As the pressure in these blood vessels increases, fluid is pushed into the air spaces (alveoli) in the lungs. This fluid reduces normal oxygen movement through the lungs. These two factors combine to cause shortness of breath.

1. What is hemodialysis?
2. Why do you do hemodialysis?
3. How does hemodialysis remove body waste?
4. What are the symptoms and side effects of hemodialysis?
5. How should I eat food when I do hemodialysis?
6. What are some precautions for patients during hemodialysis?
► If you have any health issues contact us anytime, we here to help at CloudHospital – https://icloudhospital.com/
► Subscribe: https://www.youtube.com/channel/UCmk5... to learn more about various health and beauty topics.
► Find us on Facebook: https://www.facebook.com/icloudhospital/
► On Instagram: https://www.instagram.com/cloudhospit...
► On LinkedIn: https://www.linkedin.com/company/clou...
► On Twitter: https://twitter.com/CloudhospitalI
#hemodialysis #cloudhospital #koreahospital