Top videos
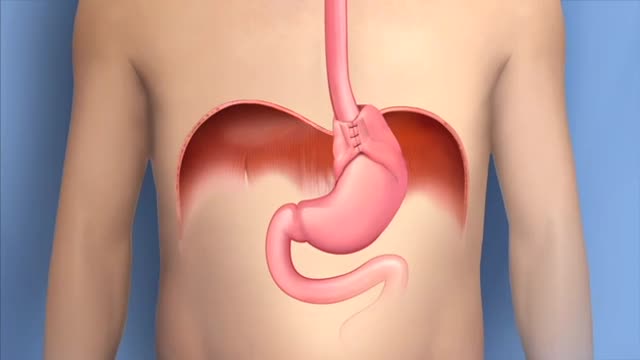
Fundoplication Surgery for Gastroesophageal Reflux Disease (GERD) Guide. During fundoplication surgery, the upper curve of the stomach (the fundus) is wrapped around the esophagus and sewn into place so that the lower portion of the esophagus passes through a small tunnel of stomach muscle.
Aplastic anemia is a hematopoietic disorder caused due to T lymphocyte mediated destruction of stem cells resulting in pancytopenia with a cellular bone marrow and normal cell cytogenetics. The causes of aplastic anaemia may be inherited or acquired. The causes and the diagnostic approach, along with spectrum of severity of this disorder is discussed in this presentation. A detailed discussion of the management options, along with pharmacological therapy and supportive therapy in these cases is also discussed. The treatment options include, in addition to a stem cell transplant, anti-thymocyte globulin, cyclosporine, methyprednisolone and eltrombopag (for patients who have failed treatment on combined modality therapy with ATG and cyclosporine)
Caesarean section is the most common way to deliver a breech baby in the USA, Australia, and Great Britain. Like any major surgery, it involves risks. Maternal mortality is increased by a Caesarean section, but still remains a rare complication in the First World. Third World statistics are dramatically different, and mortality is increased significantly. There is remote risk of injury to the mother’s internal organs, injury to the baby, and severe hemorrhage requiring hysterectomy with resultant infertility. More commonly seen are problems with noncatastrophic bleeding, postoperative infection and wound healing problems. It should be added that the increase in maternal mortality rates could be slightly skewed due to the fact that Caesarean sections are often used during high-risk pregnancies and/or when mortality is already a strong possibility.
One large study has confirmed that elective cesarean section has lower risk to the fetus and a slightly increased risk to the mother, than planned vaginal delivery of the breech however elements of the methodology used have undergone some criticism.
The same birth injuries that can occur in vaginal breech birth may rarely occur in Caesarean breech delivery. A Caesarean breech delivery is still a breech delivery. However the soft tissues of the uterus and abdominal wall are more forgiving of breech delivery than the hard bony ring of the pelvis. If a Caesarean is scheduled in advance (rather than waiting for the onset of labor) there is a risk of accidentally delivering the baby too early, so that the baby might have complications of prematurity. The mother’s subsequent pregnancies will be riskier than they would be after a vaginal birth (uterine rupture). The presence of a uterine scar will be a risk factor for any subsequent pregnancies.
Pharyngitis is caused by swelling in the back of the throat (pharynx) between the tonsils and the voice box (larynx). Most sore throats are caused by colds, the flu, coxsackie virus or mono (mononucleosis). Bacteria that can cause pharyngitis in some cases: Strep throat is caused by group A streptococcus.

A parasitic twin (also known as an asymmetrical or unequal conjoined twin) is the result of the processes that produce vanishing twins and conjoined twins, and may represent a continuum between the two. Parasitic twins occur when a twin embryo begins developing in utero, but the pair does not fully separate, and one embryo maintains dominant development at the expense of the other. Unlike conjoined twins, one ceases development during gestation and is vestigial to a mostly fully-formed, otherwise healthy individual twin. The undeveloped twin is defined as parasitic, rather than conjoined, because it is incompletely formed or wholly dependent on the body functions of the complete fetus. The independent twin is called the autosite.

Each person's knee is different. This is why UC San Diego Health offers several surgical options for knee replacements to tailor care to each person's injury and health. Each surgical approach has benefits for the right surgical candidate. Our surgeons can discuss what option is most appropriate for each person.
To learn more about knee replacement options at UC San Diego Health, visit:
https://health.ucsd.edu/specia....lties/orthopedics/jo
Francis Gonzales, MD, is a board-certified orthopedic surgeon who specializes in adult hip and knee joint replacement surgery. Learn more about Dr. Gonzales: https://providers.ucsd.edu/det....ails/11935/orthopedi
UC San Diego Health is repeatedly ranked among the nation's best in orthopedic care by U.S. News & World Report. We are also a Blue Distinction Center recognized for our treatment expertise and better overall patient results for knee replacement, as well as a designated Center of Excellence for orthopedic care by Optum. This means you'll receive expert, safe and cost-effective care.
UC San Diego Health's orthopedic surgeons are the first and only in San Diego to offer customized knee replacements with the ROSA knee system — for a faster recovery and more natural feeling knee. Talk to one of our surgeons about whether a ROSA knee replacement is right for you. https://health.ucsd.edu/specia....lties/orthopedics/jo#a

This follow-along routine features stretching and strengthening exercises for before and after knee replacement surgery. Daljit, who is awaiting knee surgery, joins physiotherapist Milly Abdullah to demonstrate the exercises.
This video is part of the Surgery Toolkit, a series designed for people living with arthritis who are awaiting or recovering from joint replacement surgery. Staying active is important if you’re waiting for or recovering from surgery. Being fitter and stronger can improve the success of the operation and lead to a faster recovery time.
In the Surgery Toolkit you’ll also find tailor-made, follow-along exercise routines for hip and shoulder replacement, as well as full body workouts to help you maintain overall fitness. The series also includes advice films, personal stories and top tips on staying active before and after surgery from those living with arthritis who have been through joint replacement surgery.
This series is part of Let’s Move, a programme for people with arthritis who want more movement in their lives. Sign up today to the free newsletter to receive all the latest content to help you to get active in a way that works for you: https://action.versusarthritis.....org/page/120448/dat

The fuel for the process leading to orgasm is testosterone, a hormone produced in steady supply by the testicles. The testicles also make millions of sperm each day, which mature and then are mixed with whitish, protein-rich fluids. These fluids nourish and support the sperm so they can live after ejaculation for a limited time. This mixture of fluid and sperm, known as semen, is what is moved through the urethra and out the penis during orgasm.

Dr. Nick demonstrates how to numb a toe for a patient who had a subungual hematoma “collection of blood under the nail”. This patient stubbed his toe and needed to have the nail removed.
#satisfying #reaction #amazing
MAKE SURE TO SUBSCRIBE FOR ALL THE NEW SURGICAL AND EDUCATIONAL VIDEOS COMING!!
👉🏻For more information visit :
https://drnickcampi.com
👉🏻Follow me on TikTok!!
https://vm.tiktok.com/ZMeXLbc5F/I’ll
👉🏻Connect with me!!
https://www.instagram.com/drnickcampitelli
👉🏻Check out this video of how we remove an ingrown toenail!
https://youtu.be/JyZo8aZDYds
👉🏻Dr. Nick Campitelli Performs latest Minimally Invasive Bunion Surgery! Watch this video!
https://youtu.be/eRpABMsCbOU
Dr. Nick Campitelli is a podiatrist who specializes in foot and ankle surgery in the Akron and Cleveland Ohio area. He is the Residency Director of the Western Reserve Hospital / University Hospital Podiatric Medicine and Surgery Residency Program.
*** All content found on the this YouTube video including: text, images, audio, or other formats were created for informational purposes only. The Content is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you heard on this video. ***
◦
Get the best medical animation videos made at https://www.b2w.tv/healthcare-video-production
Check out more animated healthcare videos from out blog here https://www.b2w.tv/blog/health....care-marketing-video
Medical device manufacturers need to find new and innovative ways to explain their products to potential buyers.
It can be difficult for potential buyers to understand how a medical device works, and even more difficult to visualize how it would be used in a clinical setting.
Medical animation videos are the perfect way to showcase your medical devices.
They are engaging, easy to understand, and help potential buyers see how your product would fit into their workflow.
Jump to the video you like:
8. Pharming Healthcare 0:09
7. ThermoFisher Scientific 2:46
6. Fibrogen 5:49
5. OrthAlign 9:29
4. Edwards LifeSciences 11:34
3. Edwards LifeSciences 12:51
2. Edwards LifeSciences 13:43
1. Edwards LifeSciences 18:14
Check out more Healthcare Videos we have made for our clients:
1. Healthcare Explainer Video for WelbeHealth: https://on.b2w.tv/3OFRaWo
2. Healthcare Product Explainer Video for Edwards Lifesciences: https://on.b2w.tv/3OSdMDb
3. Healthcare Commercial Video for Coopervision: https://on.b2w.tv/45muvpf
4. Healthcare Marketing Video for OrthAlign: https://on.b2w.tv/3P8KBgD
5. Healthcare Video Marketing with The Video-First Approach: https://on.b2w.tv/3LiNDfW
6. 12 Best Brand Archetypes for Healthcare Videos: https://on.b2w.tv/3EIQ0Vu
Want to learn more about Healthcare Videos? Check out our blogs:
1. 10 Best Healthcare Marketing Videos: https://on.b2w.tv/47LxhpJ
2. 5 Animated Healthcare Commercial Videos: https://on.b2w.tv/47IgpAd
3. 11 Animated Healthcare Explainer Videos: https://on.b2w.tv/3Zd7fYM
4. How Long Does It Take To Make an Healthcare Explainer Video: https://on.b2w.tv/45nasak
5. Script for Healthcare Explainer Videos: https://on.b2w.tv/47IY1af
6. Guide to Making Your Own Healthcare Explainer Video: https://on.b2w.tv/3P6FKMR
#medicaldevice #medicalanimation #medicalanimations

Empyema can develop after you have pneumonia. Many different types of bacteria may cause pneumonia, but the two most common are Streptococcus pneumoniae and Staphylococcus aureus. Occasionally, empyema may happen after you've had surgery on your chest. Medical instruments can transfer bacteria into your pleural cavity
http://dissolve-kidney-stones-fast.info-pro.co/ No-one knows better than me the physical pain and heartache that’s caused by kidney stones. and for many years I was a fellow sufferer of this nasty affliction. I know that many of you are experiencing an attack right now. Let me tell you -I’ve been there lots of times myself. I know what it’s like: the shooting abdominal pain that can last for hours, the nausea, the burning sensation and the constant water infections. Even when you get some temporary relief, you can never really relax. You’re always looking over your shoulder, waiting for those tell tale signs which signify another kidney stone attack on the horizon. You want to just get on with your life. But you can’t. If you’re anything like I was, you’d do anything for a cure. I decided to utilise my research skills to get to the bottom of the problem. This led me on a mission to find a safe, natural and effective method of defeating kidney stones. The good news: I found it. You too can share in this discovery and rid yourself of kidney stones – the natural way. natural remedy brings instant relief finally a permanent cure for kidney stones. click here. http://dissolve-kidney-stones-fast.info-pro.co/
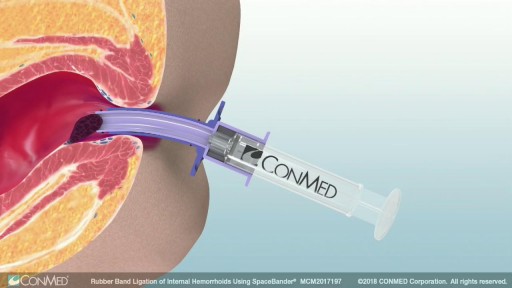
Rubber band ligation is a procedure in which the hemorrhoid is tied off at its base with rubber bands, cutting off the blood flow to the hemorrhoid. This treatment is only for internal hemorrhoids. To do this procedure, a doctor inserts a viewing instrument (anoscope) into the anus. The hemorrhoid is grasped with an instrument, and a device places a rubber band around the base of the hemorrhoid. The hemorrhoid then shrinks and dies and, in about a week, falls off. A scar will form in place of the hemorrhoid, holding nearby veins so they don't bulge into the anal canal. The procedure is done in a doctor's office. You will be asked whether the rubber bands feel too tight. If the bands are extremely painful, a medicine may be injected into the banded hemorrhoids to numb them. After the procedure, you may feel pain and have a sensation of fullness in the lower abdomen. Or you may feel as if you need to have a bowel movement. Treatment is limited to 1 to 2 hemorrhoids at a time if done in the doctor's office. Several hemorrhoids may be treated at one time if the person has general anesthesia. Additional areas may be treated at 4- to 6-week intervals.