Top videos

A fractured rib is usually a result of a fall or accident. Prolonged coughing and sports with repetitive movement, such as golf, also can cause a rib fracture. Symptoms include pain when taking a deep breath, pressing on the injured area, or bending or twisting the body. In most cases, fractured ribs usually heal on their own in one or two months. Pain relievers can make it easier to breathe deeply.
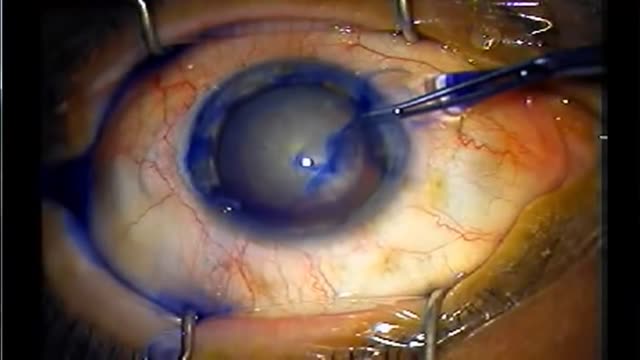
In cataract surgery, the lens inside your eye that has become cloudy is removed and replaced with an artificial lens (called an intraocular lens, or IOL) to restore clear vision. The procedure typically is performed on an outpatient basis and does not require an overnight stay in a hospital or other care facility.

Considering having an Austin plastic surgery procedure like Smartlipo? Then you’ll want to watch this quick video where staff members of renowned Austin plastic surgeon Dr. William Davis give you an overview of what you can expect.

Nasal polyps are linked to allergic rhinitis, asthma, aspirin allergy, sinus infections, acute and chronic infections, something stuck in the nose, and cystic fibrosis. But many times the cause is unknown. Sometimes, people get them before they develop asthma or sinusitis
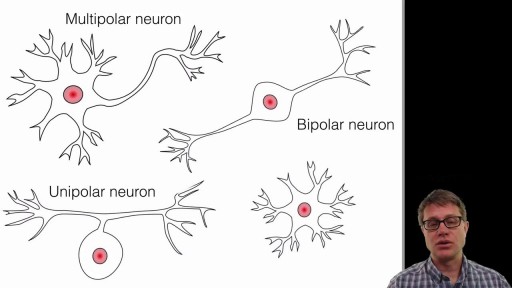
A neuron, also known as a neurone (British spelling) and nerve cell, is an electrically excitable cell that receives, processes, and transmits information through electrical and chemical signals. These signals between neurons occur via specialized connections called synapses.

Visit our website to learn more about using Nucleus animations for patient engagement and content marketing: http://www.nucleushealth.com/?utm_source=youtube&utm_medium=video-description&utm_campaign=appendect-020615
This 3D medical animation depicts the surgical removal of the appendix (appendectomy) using laparoscopic instruments. The surgery animation begins by showing an inflamed appendix (appendicitis), followed by the placement of the laparoscope. Afterward, one can see the surgical device staple, cut and remove the inflamed appendix. Following the removal of the appendix the abdomen is flushed with a sterile saline solution to ensure all traces of infection have been removed.
#laparoscopy #appendix #appendicitis
ANCE00183

The cardiac examination is one of the earliest clinical skills that medical students learn. As a junior doctor, the examination of the cardiovascular system can be almost a dreaded examination, as cardiac murmurs can literally take years of exposure in order to gain confidence with their identification through cardiac auscultation.
This video demonstrates not merely the examination of the heart, but the complete cardiovascular system including peripheries.
I hope these clinical skill revision videos are helpful, please like and subscribe and join the community so that we can create more effective videos to help with your journey through medical school
#CardiacExam #ClinicalExamination #asmr