- Physical Examination
- Surgical Examination
- Ophthalmology
- Clinical Skills
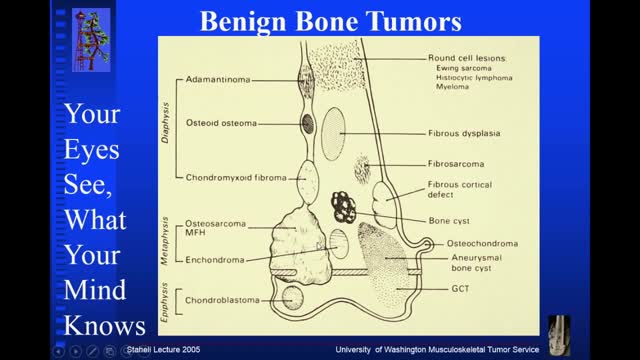
- Orthopedics
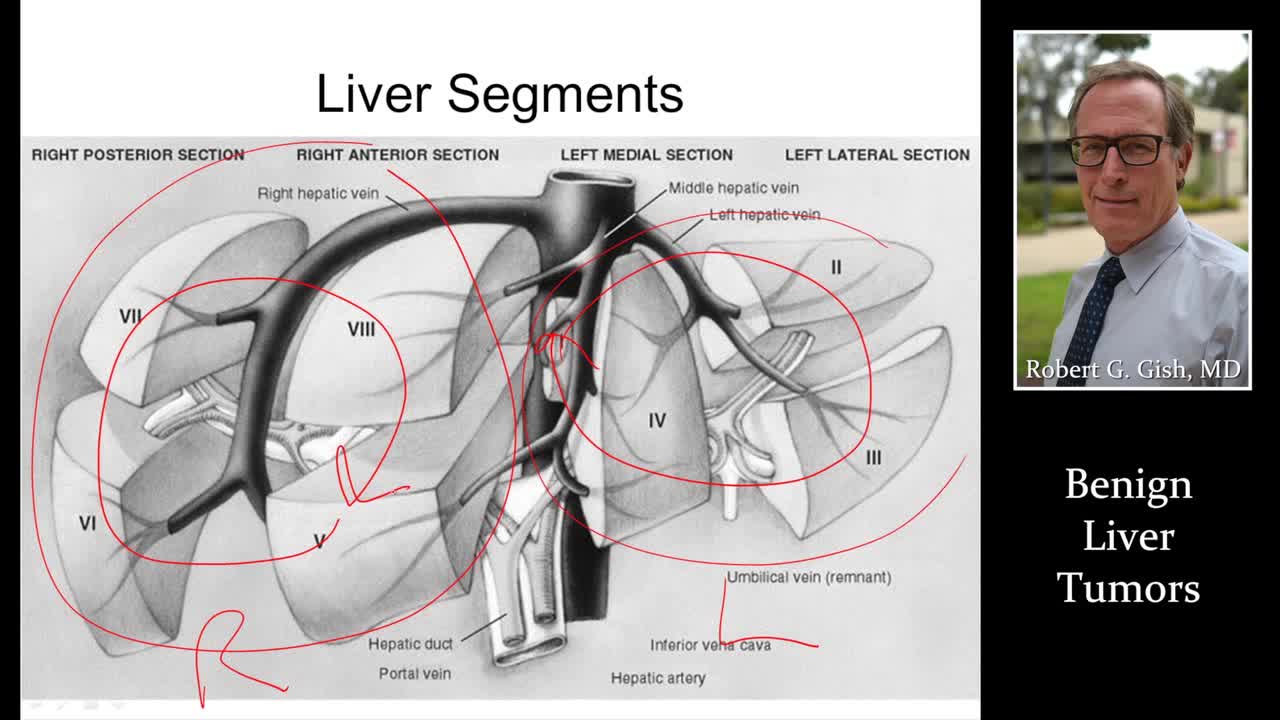
- Surgery Videos
- Laparoscopy
- Pediatrics
- Funny Videos
- Cardiothoracic Surgery
- Nursing Videos
- Plastic Surgery
- Otorhinolaryngology
- Histology and Histopathology
- Neurosurgery
- Dermatology
- Pediatric Surgery
- Urology
- Dentistry
- Oncology and Cancers
- Anatomy Videos
- Health and Fitness
- Radiology
- Anaesthesia
- Physical Therapy
- Pharmacology
- Interventional Radiology
- Cardiology
- Endocrinology
- Gynecology
- Emergency Medicine
- Psychiatry and Psychology
- Childbirth Videos
- General Medical Videos
- Nephrology
- Physiology
- Diet and Food Health
- Diabetes Mellitus
- Neurology
- Women Health
- Osteoporosis
- Gastroenterology
- Pulmonology
- Hematology
- Rheumatology
- Toxicology
- Nuclear Medicine
- Infectious Diseases
- Vascular Disease
- Reproductive Health
- Burns and Wound Healing
- Other
Benign Prostatic Hyperplasia
Benign prostatic hyperplasia (BPH), also known as benign prostatic hypertrophy, is a histologic diagnosis characterized by proliferation of the cellular elements of the prostate. Cellular accumulation and gland enlargement may result from epithelial and stromal proliferation, impaired preprogrammed cell death (apoptosis), or both. BPH involves the stromal and epithelial elements of the prostate arising in the periurethral and transition zones of the gland (see Pathophysiology). The hyperplasia presumably results in enlargement of the prostate that may restrict the flow of urine from the bladder. BPH is considered a normal part of the aging process in men and is hormonally dependent on testosterone and dihydrotestosterone (DHT) production. An estimated 50% of men demonstrate histopathologic BPH by age 60 years. This number increases to 90% by age 85 years. The voiding dysfunction that results from prostate gland enlargement and bladder outlet obstruction (BOO) is termed lower urinary tract symptoms (LUTS). It has also been commonly referred to as prostatism, although this term has decreased in popularity. These entities overlap; not all men with BPH have LUTS, and likewise, not all men with LUTS have BPH. Approximately half of men diagnosed with histopathologic BPH demonstrate moderate-to-severe LUTS. Clinical manifestations of LUTS include urinary frequency, urgency, nocturia (awakening at night to urinate), decreased or intermittent force of stream, or a sensation of incomplete emptying. Complications occur less commonly but may include acute urinary retention (AUR), impaired bladder emptying, the need for corrective surgery, renal failure, recurrent urinary tract infections, bladder stones, or gross hematuria. (See Presentation.) Prostate volume may increase over time in men with BPH. In addition, peak urinary flow, voided volume, and symptoms may worsen over time in men with untreated BPH (see Workup). The risk of AUR and the need for corrective surgery increases with age.