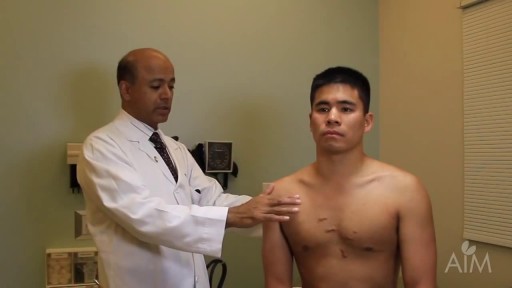
- Physical Examination
- Surgical Examination
- Ophthalmology
- Clinical Skills
- Orthopedics
- Surgery Videos
- Laparoscopy
- Pediatrics
- Funny Videos
- Cardiothoracic Surgery
- Nursing Videos
- Plastic Surgery
- Otorhinolaryngology
- Histology and Histopathology
- Neurosurgery
- Dermatology
- Pediatric Surgery
- Urology
- Dentistry
- Oncology and Cancers
- Anatomy Videos
- Health and Fitness
- Radiology
- Anaesthesia
- Physical Therapy
- Pharmacology
- Interventional Radiology
- Cardiology
- Endocrinology
- Gynecology
- Emergency Medicine
- Psychiatry and Psychology
- Childbirth Videos
- General Medical Videos
- Nephrology
- Physiology
- Diet and Food Health
- Diabetes Mellitus
- Neurology
- Women Health
- Osteoporosis
- Gastroenterology
- Pulmonology
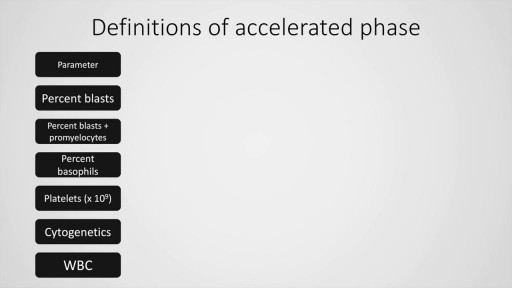
- Hematology
- Rheumatology
- Toxicology
- Nuclear Medicine
- Infectious Diseases
- Vascular Disease
- Reproductive Health
- Burns and Wound Healing
- Other
Chronic Inflammatory Demyelinating Polyneuropathy
The term chronic inflammatory demyelinating polyradiculoneuropathy (CIDP) has been used to identify patients with a chronically progressive or relapsing symmetric sensorimotor disorder with cytoalbuminologic dissociation and interstitial and perivascular endoneurial infiltration by lymphocytes and macrophages. It can be considered the chronic equivalent of acute inflammatory demyelinating polyradiculoneuropathy, the most common form of Guillain-Barré syndrome. Signs and symptoms CIDP typically starts insidiously and evolves slowly, in either a slowly progressive or a relapsing manner, with partial or complete recovery between recurrences; periods of worsening and improvement usually last weeks or months. Most experts consider the necessary duration of symptoms to be greater than 8 weeks for the diagnosis of CIDP to be made. Symptoms reported include the following: Preceding infection (infrequent) Initial limb weakness, both proximal and distal Sensory symptoms (eg, tingling and numbness of hands and feet) Motor symptoms (usually predominant) In about 16% of patients, a relatively acute or subacute onset of symptoms In children, usually a more precipitous onset of symptoms Symptoms of autonomic system dysfunction (eg, orthostatic dizziness) Pertinent physical findings are limited to the nervous system, except when the condition is associated with other diseases. Such findings may include the following. Signs of cranial nerve (CN) involvement (eg, facial muscle paralysis or diplopia) Gait abnormalities Motor deficits (eg, symmetric weakness of both proximal and distal muscles in upper and lower extremities) Diminished or absent deep tendon reflexes Sensory deficits (typically in stocking-glove distribution) Impaired coordination See Clinical Presentation for more detail. Diagnosis Laboratory studies that may be helpful include the following: Cerebrospinal fluid analysis: Elevated protein levels are common (80% of patients); 10% of patients also have mild lymphocytic pleocytosis and increased gamma globulin Complete blood count (CBC), erythrocyte sedimentation rate (ESR), antinuclear antibody (ANA) level, biochemistry profile, and serum and urine immunoelectrophoresis (to exclude associated systemic disorders) In certain instances, genetic testing Other tests and procedures that may be warranted are as follows: MRI of the spine with gadolinium enhancement Electromyography (EMG) is a critical test to determine whether the disorder is truly a peripheral neuropathy and whether the neuropathy is demyelinating Peripheral (sural) nerve biopsy (see the image below): This is considered when the diagnosis is not completely clear, when other causes cannot be excluded, or when profound axonal involvement is observed on EMG; biopsy was once commonly recommended for most patients before immunosuppressive therapy, but current guidelines no longer recommend it