chronic obstructive pulmonary disease
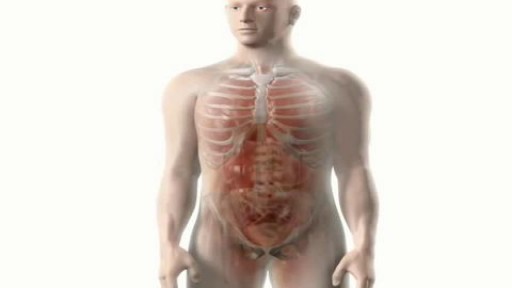
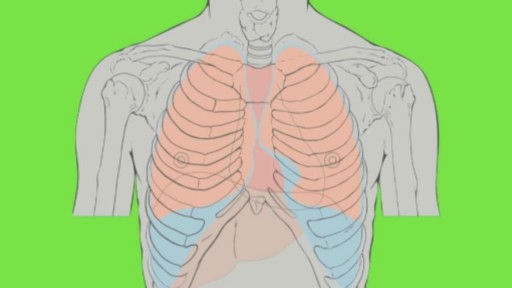
Pathologic changes in chronic obstructive pulmonary disease (COPD) occur in the large (central) airways, the small (peripheral) bronchioles, and the lung parenchyma. Most cases of COPD are the result of exposure to noxious stimuli, most often cigarette smoke. The normal inflammatory response is amplified in persons prone to COPD development. The pathogenic mechanisms are not clear but are most likely diverse. Increased numbers of activated polymorphonuclear leukocytes and macrophages release elastases in a manner that cannot be counteracted effectively by antiproteases, resulting in lung destruction. The primary offender has been found to be human leukocyte elastase, with synergistic roles suggested for proteinase-3 and macrophage-derived matrix metalloproteinases (MMPs), cysteine proteinases, and a plasminogen activator. Additionally, increased oxidative stress caused by free radicals in cigarette smoke, the oxidants released by phagocytes, and polymorphonuclear leukocytes all may lead to apoptosis or necrosis of exposed cells. Accelerated aging and autoimmune mechanisms have also been proposed as having roles in the pathogenesis of COPD.[5, 6] Cigarette smoke causes neutrophil influx, which is required for the secretion of MMPs; this suggests, therefore, that neutrophils and macrophages are required for the development of emphysema. Studies have also shown that in addition to macrophages, T lymphocytes, particularly CD8+, play an important role in the pathogenesis of smoking-induced airflow limitation. To support the inflammation hypothesis further, a stepwise increase in alveolar inflammation has been found in surgical specimens from patients without COPD versus patients with mild or severe emphysema. Indeed, mounting evidence supports the concept that dysregulation of apoptosis and defective clearance of apoptotic cells by macrophages play a prominent role in airway inflammation, particularly in emphysema.[7] Azithromycin (Zithromax) has been shown to improve this macrophage clearance function, providing a possible future treatment modality.[8] In patients with stable COPD without known cardiovascular disease, there is a high prevalence of microalbuminuria, which is associated with hypoxemia independent of other risk factors.[9] Chronic bronchitis Mucous gland hyperplasia (as seen in the images below) is the histologic hallmark of chronic bronchitis. Airway structural changes include atrophy, focal squamous metaplasia, ciliary abnormalities, variable amounts of airway smooth muscle hyperplasia, inflammation, and bronchial wall thickening.