- Physical Examination
- Surgical Examination
- Ophthalmology
- Clinical Skills
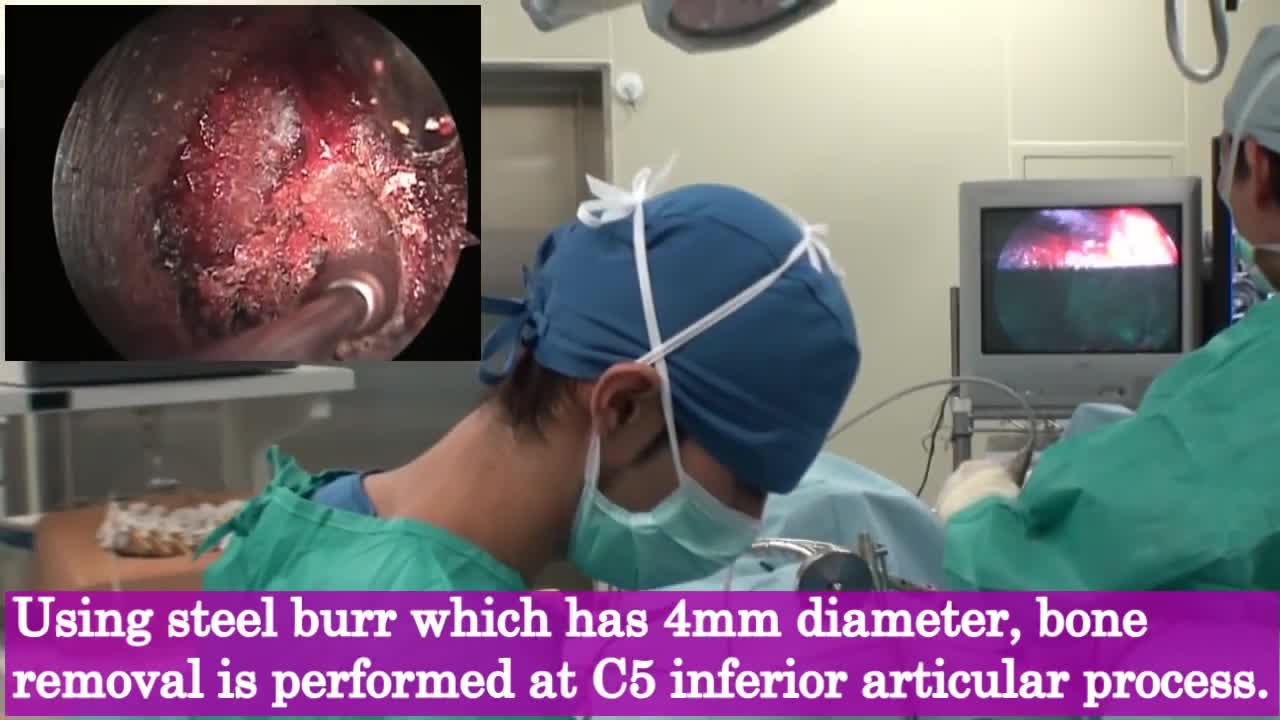
- Orthopedics
- Surgery Videos
- Laparoscopy
- Pediatrics
- Funny Videos
- Cardiothoracic Surgery
- Nursing Videos
- Plastic Surgery
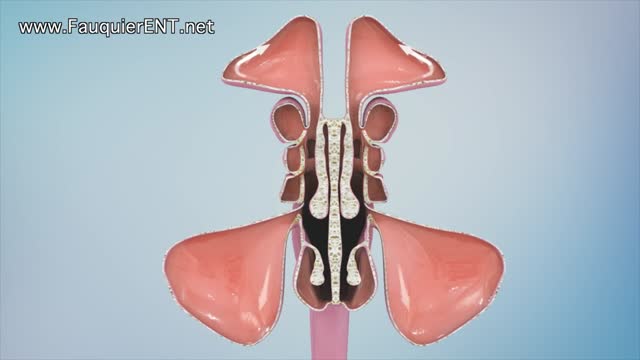
- Otorhinolaryngology
- Histology and Histopathology
- Neurosurgery
- Dermatology
- Pediatric Surgery
- Urology
- Dentistry
- Oncology and Cancers
- Anatomy Videos
- Health and Fitness
- Radiology
- Anaesthesia
- Physical Therapy
- Pharmacology
- Interventional Radiology
- Cardiology
- Endocrinology
- Gynecology
- Emergency Medicine
- Psychiatry and Psychology
- Childbirth Videos
- General Medical Videos
- Nephrology
- Physiology
- Diet and Food Health
- Diabetes Mellitus
- Neurology
- Women Health
- Osteoporosis
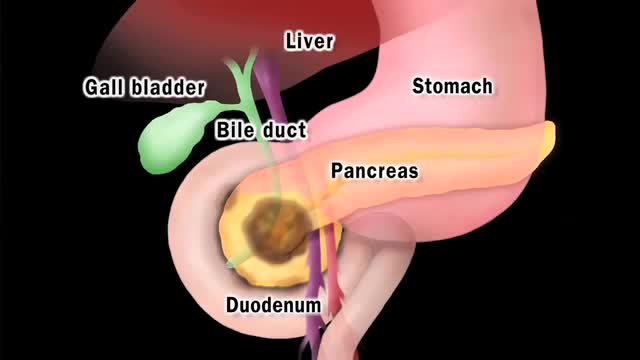
- Gastroenterology
- Pulmonology
- Hematology
- Rheumatology
- Toxicology
- Nuclear Medicine
- Infectious Diseases
- Vascular Disease
- Reproductive Health
- Burns and Wound Healing
- Other
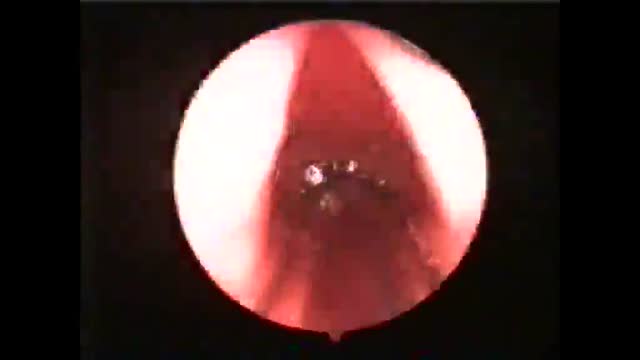
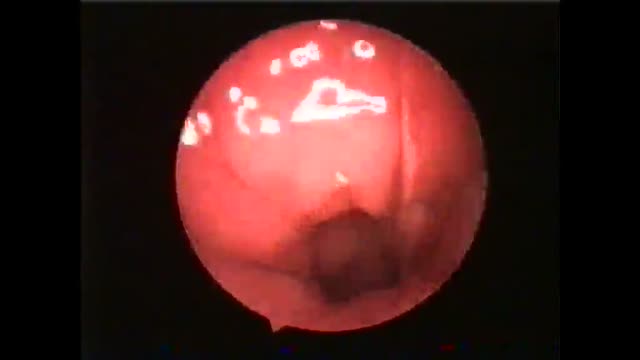
Endoscopic Transgastric Pancreatic Necrosectomy
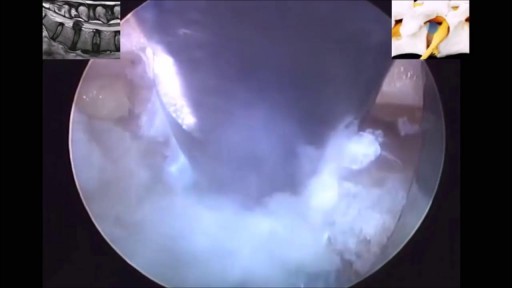
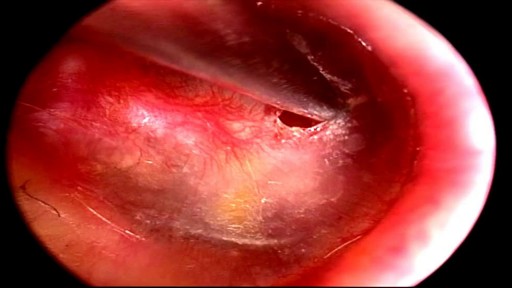
We herein describe endoscopic treatment of symptomatic pancreatic pseudocyst with significant necrosis and a fistula. Fifty eight year old man had presented to us with a large pseudocyst following an episode of acute pancreatitis. He was complaining of significant abdominal pain for two months. A... CT scan abdominal had revealed a large retro-gastric pseudocyst with necrosis and portal venous thrombosis. An upper GI endoscopy had revealed small linear fundal varcies. Endoscopic as well as surgical treatment for the cyst was discussed with the patient. Patient wished not to undergo surgical treatment and therefore endoscopic treatment was selected after a proper consent. EUS was performed to see for the interposed vessel prior to the pseudocyst puncture. Needle knife puncture was made and a guide wire was passed in the pseudocyst cavity. After confirming the wire placement in the cyst, the tract was dilated up to 20 mms using a CRE balloon. Fluid from the cyst was emptied out in the stomach. An ERCP scope was passed in to the cyst cavity, which revealed a significant necrotic material (much more than what the CT scan had revealed). All the free lying necrotic material was taken out with the help of a snare and a dormia basket. A lot of necrotic was stuck to the cyst wall, which was removed with the help of water jet, mechanical scooping and cutting through using a needle knife papillotome. Three 10 fr. Pigtail stents were placed at the end of the procedure. Further necrosectomy was carried out on alternate days for three more sessions. Dilation was required prior to each session three pigtail trans-gastric stents were placed at the end of each session. Single stent was kept in situ during each procedure to guide the path (the position of the stoma changed dramatically once the cyst was empty). During the last lesion (session four), a pancreatogram was taken. It revealed a mildly dilated CBD in the head, normally duct in the proximal body with a leak from the distal body, and contrast was seen going in to the pseudocyst cavity. The duct could not be opacified distally. A 7 fr. 15 cms stent was placed trans-papillary. When the cyst cavity was reentered through trans-gastric route, the trans-papillary pancreatic stent was clearly visible with soft necrotic material around it. In fact, the stent guided further necrosis removal. It also helped in diverting the pancreatic juice to the duodenum rather than in the pseudocyst cavity. Patient was discharged after this session and was followed up regularly. A CT scan was obtained after three months, which revealed a complete resolution of the necrosis and pseudocyst. There was a possibility of a persistent fistula after the removal of trans-papillary stent and a recurrence of the pseudocyst. Fistula closure with cyanoacrylate glue is well described in the literature. The procedure can have obvious complications secondary to accidental blockage of the main pancreatic duct. So, we thought it prudent to use a safer alternative to treat the condition. We removed the longer pancreatic stent and replaced it with a shorter pancreatic stent occupying only the head region. The patient was followed up after a month; sonography of the abdomen did not reveal any recurrence of the pseudocyst. All the stents were removed at this examination.