- Physical Examination
- Surgical Examination
- Ophthalmology
- Clinical Skills
- Orthopedics
- Surgery Videos
- Laparoscopy
- Pediatrics
- Funny Videos
- Cardiothoracic Surgery
- Nursing Videos
- Plastic Surgery
- Otorhinolaryngology
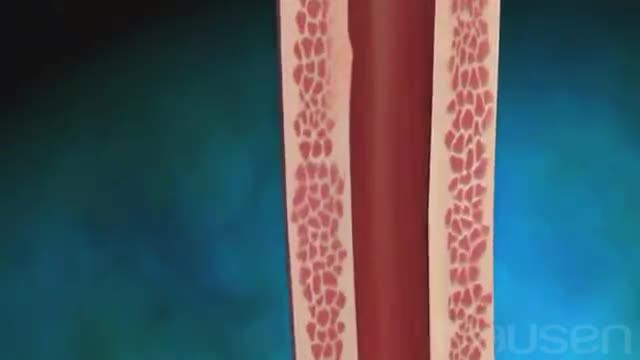
- Histology and Histopathology
- Neurosurgery
- Dermatology
- Pediatric Surgery
- Urology
- Dentistry
- Oncology and Cancers
- Anatomy Videos
- Health and Fitness
- Radiology
- Anaesthesia
- Physical Therapy
- Pharmacology
- Interventional Radiology
- Cardiology
- Endocrinology
- Gynecology
- Emergency Medicine
- Psychiatry and Psychology
- Childbirth Videos
- General Medical Videos
- Nephrology
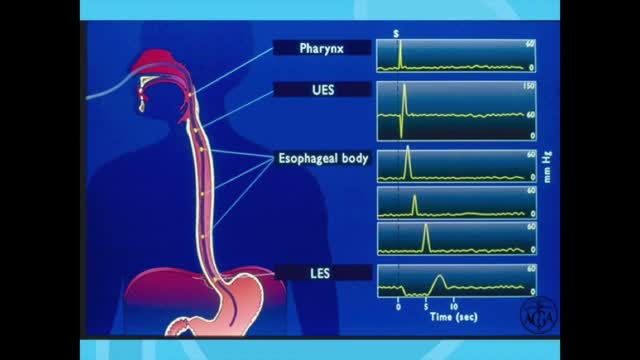
- Physiology
- Diet and Food Health
- Diabetes Mellitus
- Neurology
- Women Health
- Osteoporosis
- Gastroenterology
- Pulmonology
- Hematology
- Rheumatology
- Toxicology
- Nuclear Medicine
- Infectious Diseases
- Vascular Disease
- Reproductive Health
- Burns and Wound Healing
- Other
Esophageal En Bloc Mucosectomy
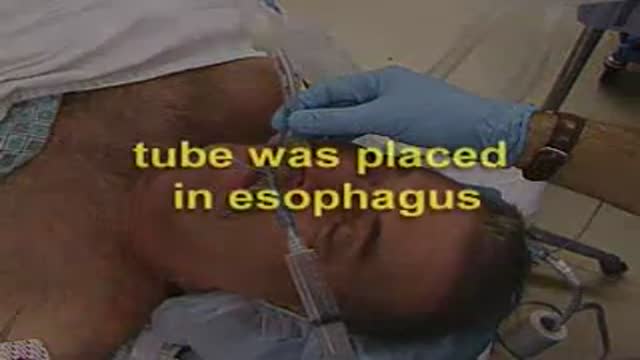
En Bloc Esophageal Mucosectomy, an experimental technique for the endolumenal management of Barrett's related dysplasia and neoplasia. High grade dysplasia is in indication for esophagectomy; however esophagectomy has a mortality rate up to 12 percent, and up to 56 percent of patients may develop s...erious post-operative complications. Multiple ablated lesions can progress under the neo-squamous layer, leading to buried Barrett's mucosa. With conventional piecemeal EMR, cautery effect limits evaluation in areas of interest, Barrett's epithelium is left behind, tissue is not evaluated in situ and invasive lesions may be missed due to incomplete sampling. A new technique, en bloc esophageal mucosectomy, or EEM, was developed. The technique begins with conventional EMR in the proximal esophagus to access the submucosal space. Conventional EMR is being performed here. The mucosa is resected using an electrothermal snare. The mucosal defect from the first EMR is seen here. EMR is then repeated on the opposing wall. Sequential EMR creates a complete concentric mucosal defect. In the following sequence the completely detached column of mucosa can be seen, bounded by submucosa and muscularis propria layers. Here in the stomach, the endoscope is retroflexed and is covered by a sleeve of esophageal mucosa which has been freed to the GE junction and inverted. This sequence demonstrates a double snare technique. This snare is alongside the endoscope. The snare has been passed through the working channel. The working channel snare is pulled back, and the snare alongside the scope is used to grasp the mucosal column. With tension on the column the working channel snare can be threatened and advanced. This sequence shows the snare as it is being passed down to the GE junction. At the GE junction, the snare is tightened and cautery is applied. This frees the column of mucosal tissue from the remaining attachment. The endoscope is then withdrawn. Then detached mucosal column can be grasped with a snare and retrieved. In the following sequence, the long column of mucosa is being withdrawn via the overtube. Here, endoscopic forceps have been passed through the column to demonstrates the concentric nature of the specimen. The length of mucosa can be seen here alongside 2 conventional EMR specimens. Approximately 15cm of tissues was removed in this case. On endoscopy immediately following the resection, there is no bleeding or evidence of perforation in the area of resection. The endoscope is advanced and the exposed submucosa can be appreciated down to the GE junction. This is the low power view of the histologic specimen generated by EEM. Metaplastic tissue adjacent to a dysplastic focus would be completely removed. With a high power view, the layers of the esophagus can be appreciated. The epithelium, lamina propria, muscularis mucosa and submucosa are visible, with no cautery artifact in the area of interest. The technique would remove metplasia, low grade dysplasia, high grade dysplasia, and intramucosal carcinoma, as well a T 1 a lesions. All the animals in this series tolerated the procedure well. A total of five non-survival procedures and 4 survival procedures were performed. In the survival procedures, all four swine thrived in the post-operative period. Two swine were then survived for 9 days following the procedure. On post —op day nine, after passing into the upper esophagus, the proximal margin of the mucosectomy is seen here. Healing appears to be occurring. There is no evidence of leak, and no stricting is seen at 9 days down to the GE junction Passing into the stomach, some residual feed can be seen. Two swine were then survived for 13 days. On this follow-up endoscopy, the area of the mucosectomy is again healing. There was a loose stricture in both animals and both were easily traversed with a 9.8 mm gastroscope. There was a gross appearance of re-epitheliazation in some areas. It is notable that the stricture was present in the proximal esophagus with no narrowing distally. At necropsy there was not eviden