- Physical Examination
- Surgical Examination
- Ophthalmology
- Clinical Skills
- Orthopedics
- Surgery Videos
- Laparoscopy
- Pediatrics
- Funny Videos
- Cardiothoracic Surgery
- Nursing Videos
- Plastic Surgery
- Otorhinolaryngology
- Histology and Histopathology
- Neurosurgery
- Dermatology
- Pediatric Surgery
- Urology
- Dentistry
- Oncology and Cancers
- Anatomy Videos
- Health and Fitness
- Radiology
- Anaesthesia
- Physical Therapy
- Pharmacology
- Interventional Radiology
- Cardiology
- Endocrinology
- Gynecology
- Emergency Medicine
- Psychiatry and Psychology
- Childbirth Videos
- General Medical Videos
- Nephrology
- Physiology
- Diet and Food Health
- Diabetes Mellitus
- Neurology
- Women Health
- Osteoporosis
- Gastroenterology
- Pulmonology
- Hematology
- Rheumatology
- Toxicology
- Nuclear Medicine
- Infectious Diseases
- Vascular Disease
- Reproductive Health
- Burns and Wound Healing
- Other
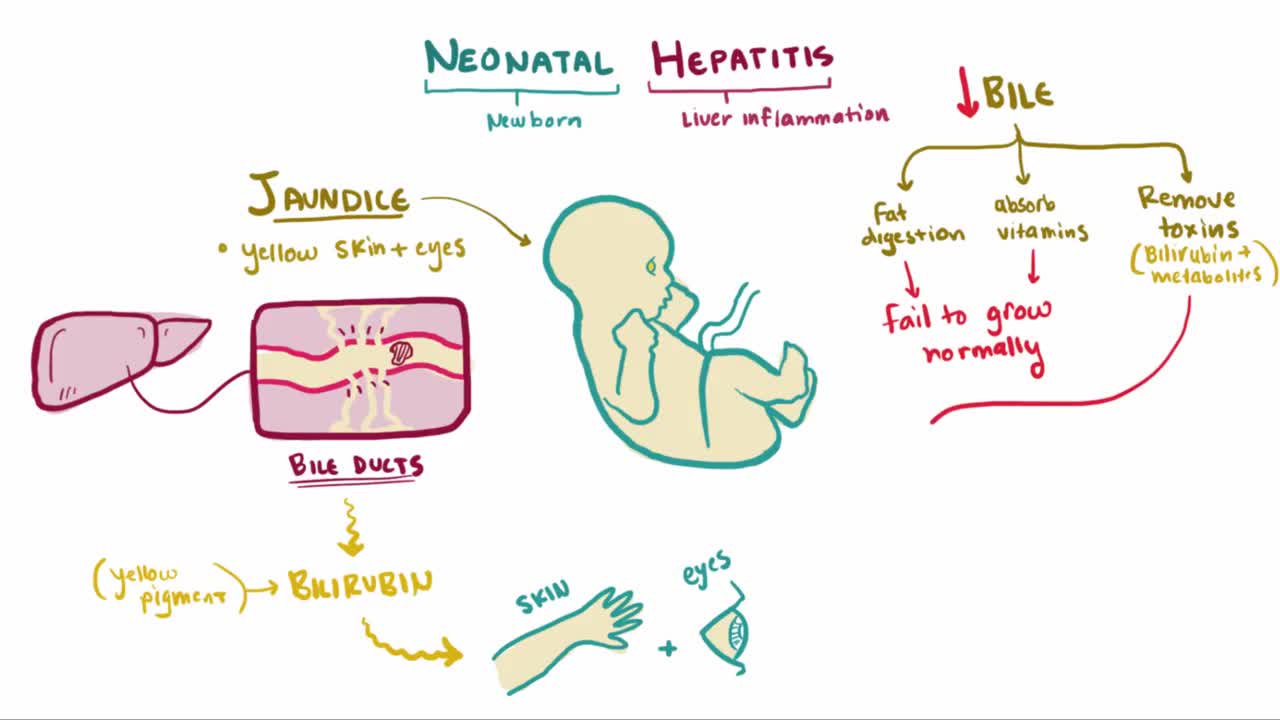
Hepatitis E
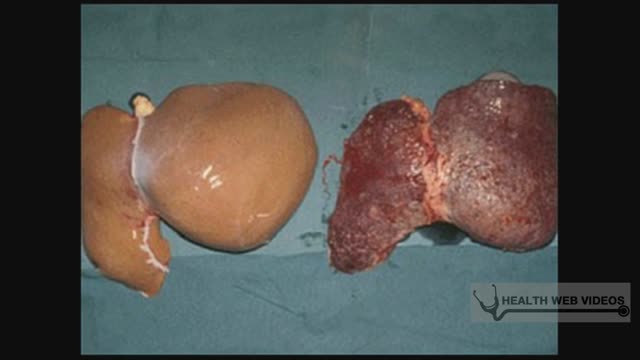
The hepatitis E virus, responsible for major epidemics of viral hepatitis in subtropical and tropical countries, was cloned only 7 years ago.1 Hepatitis E was found to belong to the family of Caliciviridae, which includes the Norwalk virus—a common cause of gastroenteritis in humans—and consists of a single, plus-strand RNA genome of approximately 7.2 kb without an envelope (Fig. 1). The virus contains at least three open reading frames encoding viral proteins against which antibodies are made on exposure. These antibodies, especially those against the capsid protein derived from the second open reading frame2 and a protein of unknown function derived from the third open reading frame, are detected by currently available serologic assays. Retrospective studies on stored sera of past epidemics of viral hepatitis in Mexico, Africa, Afghanistan, Pakistan, India, Bangladesh, Burma, Nepal, and Borneo have revealed that all were caused by strains of hepatitis E. In addition, hepatitis E was found to be responsible for the hepatitis epidemic in the southern part of Xinjiang, China, in which 120,000 persons became infected between September 1986 and April 1988.3 Hepatitis E predominantly affects young adults (15 to 40 years old). The symptoms of hepatitis E are similar to those of hepatitis A. Frequently, a prodrome consisting of anorexia, nausea, low-grade fever, and right upper abdominal pain is present 3 to 7 days before jaundice develops. Aminotransferase levels peak (usually between 1,000 and 2,000 U/L) near the onset of symptoms; bilirubin levels (10 to 20 mg/dL) peak later. Jaundice usually resolves after 1 to 2 weeks. In about 10% of cases, the disease is fulminant—especially in pregnant women, among whom mortality rates as high as 20% due to hemorrhagic and thrombotic complications have been reported. No evidence has suggested that hepatitis E can cause chronic infection. Transmission is by the fecal-oral route, predominantly through fecally contaminated drinking water supplies. In addition, however, preliminary reports have suggested transmission of the hepatitis E virus through blood transfusions. Volunteer studies confirmed the presence of the virus in serum and feces before and during clinical disease.4 The virus is shed into feces approximately 1 week before symptoms develop. The incubation period varies from 2 to 9 weeks (mean duration, approximately 45 days). Until now, a few reports had described symptomatic hepatitis E acquired in Europe;5, 6 all patients with symptomatic hepatitis E in the United States were travelers returning from Mexico, Africa, or the Far East, in whom hepatitis E developed after their return home.7 In this issue of the Mayo Clinic Proceedings (pages 1133 to 1136), Kwo and associates describe a case of hepatitis E in a man who had not left the United States during the previous 10 years. Specific serologic tests for hepatitis E virus IgG (enzyme immunoassays and a fluorescent antibody blocking assay) and IgM8 (US strain-specific enzyme-linked immunosorbent assay with use of synthetic polypeptides deduced from the viral genome, as shown in Figure 1), developed at Abbott Laboratories (IgG and IgM) as well as at the Centers for Disease Control and Prevention (IgG), were used to prove that the patient indeed had acute hepatitis E. Researchers at Abbott Laboratories have prepared a report that describes most of the viral genome in this patient (Fig. I).8 Their results are interesting because this strain from the United States differs considerably from hepatitis E strains isolated in Mexico, Burma, Pakistan, or China. Furthermore, the sequence of the US strain is highly homologous (98% and 94% homology at the amino acid level to the second and third open reading frames, respectively) to a recently isolated hepatitis E strain from American swine.9 This finding suggests that, in the United States, hepatitis E is a zoonosis with the swine population as one of its hosts. This relationship would confirm earlier studies in Asia, where swine were also found to carry variants of the hepatitis E virus.10 Why are these two recent discoveries important for medicine in the United States? First, other sporadic, locally acquired cases of acute hepatitis may be caused by hepatitis E. Second, these back-to-back discoveries strongly suggest that a common natural host for hepatitis E is present in countries with more moderate climates. Because swine do not seem to experience any symptoms associated with infection and because symptoms in humans can be minor or absent, we now may also have an explanation for the 1 to 2% of positive hepatitis E serologic results in blood donors in the United States,11 Netherlands,12 and Italy,6 countries with large swine staples. Clearly, more research needs to be done to confirm this hypothesis. Third, in countries with more moderate climates, hepatitis E may often result in a subclinical infection. Is this variation in manifestation due to less virulent strains, and do sequence variations determine virulence? Fourth, swine may be used as an animal model for study of the disease as well as vaccine development.