- Physical Examination
- Surgical Examination
- Ophthalmology
- Clinical Skills
- Orthopedics
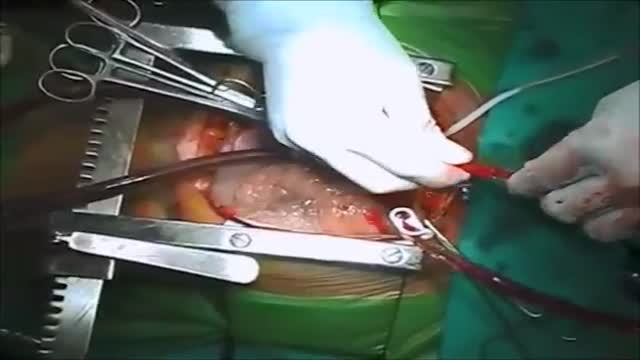
- Surgery Videos
- Laparoscopy
- Pediatrics
- Funny Videos
- Cardiothoracic Surgery
- Nursing Videos
- Plastic Surgery
- Otorhinolaryngology
- Histology and Histopathology
- Neurosurgery
- Dermatology
- Pediatric Surgery
- Urology
- Dentistry
- Oncology and Cancers
- Anatomy Videos
- Health and Fitness
- Radiology
- Anaesthesia
- Physical Therapy
- Pharmacology
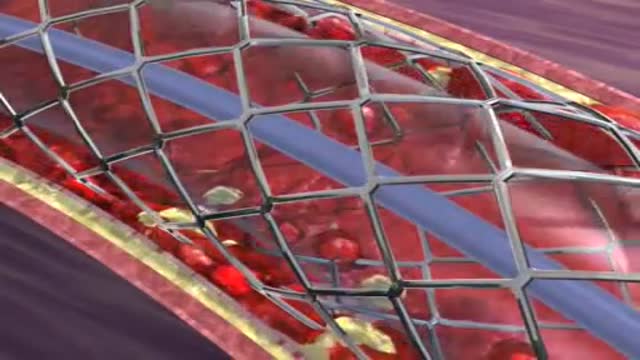
- Interventional Radiology
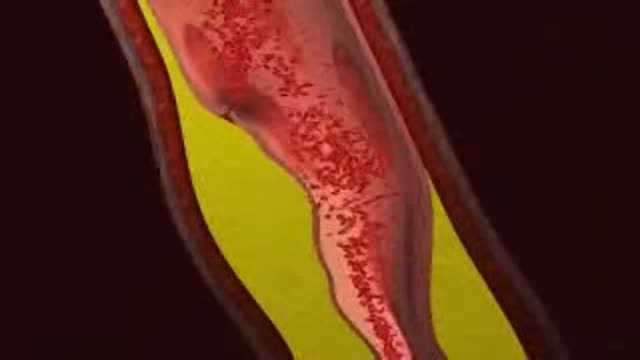
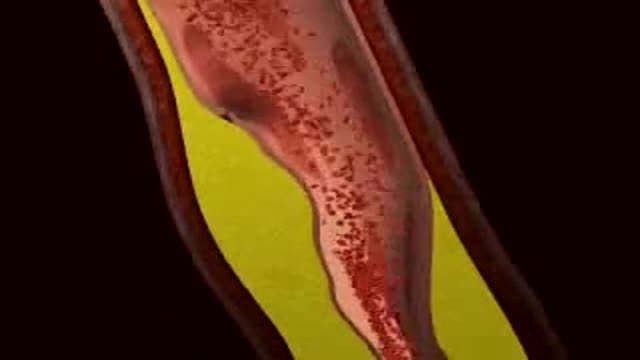
- Cardiology
- Endocrinology
- Gynecology
- Emergency Medicine
- Psychiatry and Psychology
- Childbirth Videos
- General Medical Videos
- Nephrology
- Physiology
- Diet and Food Health
- Diabetes Mellitus
- Neurology
- Women Health
- Osteoporosis
- Gastroenterology
- Pulmonology
- Hematology
- Rheumatology
- Toxicology
- Nuclear Medicine
- Infectious Diseases
- Vascular Disease
- Reproductive Health
- Burns and Wound Healing
- Other
Infarction
The occurrence and extent of cerebral infarction is determined by three basic factors: i) site of arterial occlusion, ii) the rapidity of arterial occlusion, and iii) the presence or absence of collateral circulation. Grossly, infarcts are usually divided into pale (non-hemorrhagic) and hemorrhagic types. Infarcts evolve over time, thus their gross appearance gives a clue to when they occurred. The temporal evolution of an infarct occurs in three stages: i) acute (1 day – 1 week) – the involved area is soft and edematous and there is a blurring of anatomic detail; ii) subacute (1 week – 1 month) – there is obvious tissue destruction and liquefactive necrosis of the involved brain; iii) chronic (>1 month) – the damaged tissue has been phagocytized and there is cavition with surrounding gliosis. Microscopically there is also a temporal evolution of cerebral infarcts. During the earliest phase of infarction (0-48 hours) chromatolysis and swollen eosinophilic neurons are seen. Neuronal cell necrosis and an acute inflammatory response are usually seen from 24-72 hours. This response is typically followed by an influx of mononuclear cells which begin to phagocytize necrotic debris (3-5 days). From 1-2 weeks after the infarct there is vascular proliferation and reactive astrocytosis. Over time (>1 month) the necrotic tissue will be completely removed and a cystic cavity surrounded by a glial scar will be formed.