- Physical Examination
- Surgical Examination
- Ophthalmology
- Clinical Skills
- Orthopedics
- Surgery Videos
- Laparoscopy
- Pediatrics
- Funny Videos
- Cardiothoracic Surgery
- Nursing Videos
- Plastic Surgery
- Otorhinolaryngology
- Histology and Histopathology
- Neurosurgery
- Dermatology
- Pediatric Surgery
- Urology
- Dentistry
- Oncology and Cancers
- Anatomy Videos
- Health and Fitness
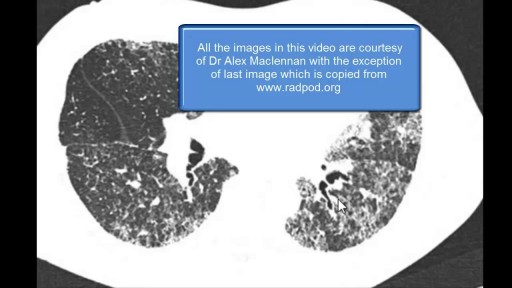
- Radiology
- Anaesthesia
- Physical Therapy
- Pharmacology
- Interventional Radiology
- Cardiology
- Endocrinology
- Gynecology
- Emergency Medicine
- Psychiatry and Psychology
- Childbirth Videos
- General Medical Videos
- Nephrology
- Physiology
- Diet and Food Health
- Diabetes Mellitus
- Neurology
- Women Health
- Osteoporosis
- Gastroenterology
- Pulmonology
- Hematology
- Rheumatology
- Toxicology
- Nuclear Medicine
- Infectious Diseases
- Vascular Disease
- Reproductive Health
- Burns and Wound Healing
- Other
interstitial cystitis
Interstitial cystitis is a clinical syndrome characterized by daytime and nighttime urinary frequency, urgency, and pelvic pain of unknown etiology. Interstitial cystitis has no clear etiology or pathophysiology, and diagnostic criteria for the syndrome remain undefined. Despite considerable research, universally effective treatments do not exist; therapy usually consists of various supportive, behavioral, and pharmacologic measures. Surgical intervention is rarely indicated. The International Continence Society has coined the term painful bladder syndrome (suprapubic pain with bladder filling associated with increased daytime and nighttime frequency, in the absence of proven urinary infection or other obvious pathology) and reserves the diagnosis of interstitial cystitis for patients with characteristic cystoscopic and histologic features of the condition.[1] An international consensus panel was able to generally agree on the following definition of interstitial cystitis/bladder pain syndrome (IC/BPS): unpleasant sensation (pain, pressure, discomfort) perceived to be related to the urinary bladder and associated with lower urinary tract symptoms of more than 6 weeks duration, in the absence of infection or other identifiable causes. American Urological Association (AUA) guidelines published in 2011 and amended in 2014 use an evidence-based approach to provide a clinical framework for the diagnosis and management of this condition.[2, 3, 4] In 1887, Skene initially described a condition characterized by inflammation that destroyed the urinary bladder "mucous membrane partly or wholly and extended to the muscular parietes." Guy Hunner popularized the disease with the description of characteristic bladder wall ulcers in association with a symptom complex of chronic bladder inflammation.[5] The first comprehensive epidemiologic description of interstitial cystitis is credited to Hand, who in 1949 described the widespread, small, submucosal bladder hemorrhages and the significant variation in bladder capacity characteristic of the condition. Despite years of intensive research, there are no specific clinical or urinary markers currently clinically available; no absolutely specific radiographic, laboratory, or serologic findings; and no biopsy patterns that are pathognomonic for interstitial cystitis. Some research suggests that the following may all play a role in the disease pathophysiology: (1) pelvic floor dyfunction, (2) dysregulated immune or inflammatory signals, (3) neural hypersensitivity, and (4) disruption of the proteoglycan/glycosaminoglycan (GAG) layer.[6] Interstitial cystitis, howerver, remains a diagnosis of exclusion (see Presentation, DDx, and Workup.) Intensive study has been done to attempt to identify biomarkers for IC/BPS. Some interesting studies have shown that bladder nitric oxide is an accurate marker for Hunner lesions, but these are not present in all patients, and the test requires specific equipment, which has limited widespread clinical use.[7] Differences in levels of cytokines and chemokines, specifically CXCL-10, have shown some ability to differentiate patients with and without Hunner lesions.[8] Other studies of ulcerative IC/BPS have shown that numerous other cytokines and chemokines are up-regulated as well, heralding a possible urinary test to identify patients.[9] An additional substance shown to be up-regulated in IC/BPS patients is antiproliferative factor (APF). This small 8–amino-acid peptide has been associated with suppression of cell growth, increases in transcellular permeability, and lowering of levels of proteins that form intercellular junctional complexes. It is synthesized and secreted from bladder epithelial cells from patients with IC/BPS and may play a key role in pathophysiology.[10] In vitro studies have shown that removal of APF from cell culture media restored cell proliferation and membrane integrity.[11] Studies have also suggested APF in the therapeutic effect of hydrodistension in patients with IC/BPS, although further confirmatory studies are necessary.[12] The most important element in treating patients with interstitial cystitis is education and emotional support. Periodic exacerbations are managed as they occur because no long-term therapy has been shown to prevent or delay recurrent episodes. Therefore, the purpose of treatment is to palliate and alleviate symptoms. Because no discrete pathognomonic pathologic criteria exist for assessing and monitoring disease severity, indications and goals for treatment are based on the degree of patient symptoms. Assessing patient response to treatment is also complicated because of the subjective nature of symptoms; the waxing and waning nature of symptoms without treatment; and the lack of objective serologic, physical, or histopathologic findings. Conservative measures and oral or intravesical treatments are considered first-line treatment. (See Treatment.)