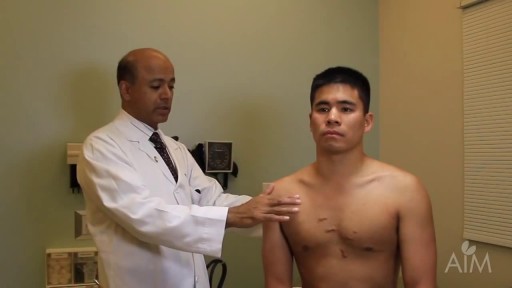
- Physical Examination
- Surgical Examination
- Ophthalmology
- Clinical Skills
- Orthopedics
- Surgery Videos
- Laparoscopy
- Pediatrics
- Funny Videos
- Cardiothoracic Surgery
- Nursing Videos
- Plastic Surgery
- Otorhinolaryngology
- Histology and Histopathology
- Neurosurgery
- Dermatology
- Pediatric Surgery
- Urology
- Dentistry
- Oncology and Cancers
- Anatomy Videos
- Health and Fitness
- Radiology
- Anaesthesia
- Physical Therapy
- Pharmacology
- Interventional Radiology
- Cardiology
- Endocrinology
- Gynecology
- Emergency Medicine
- Psychiatry and Psychology
- Childbirth Videos
- General Medical Videos
- Nephrology
- Physiology
- Diet and Food Health
- Diabetes Mellitus
- Neurology
- Women Health
- Osteoporosis
- Gastroenterology
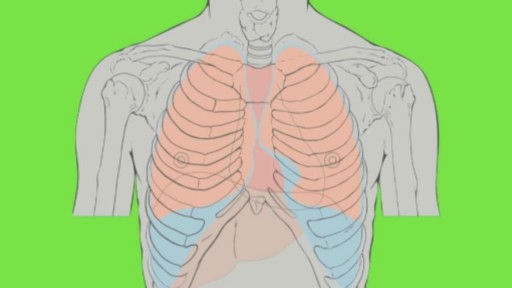
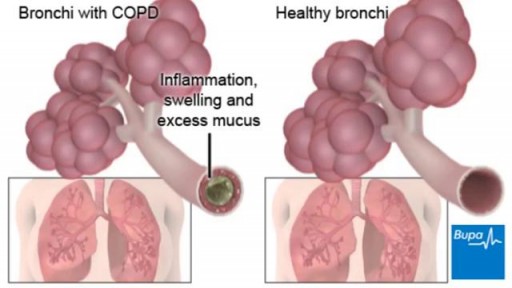
- Pulmonology
- Hematology
- Rheumatology
- Toxicology
- Nuclear Medicine
- Infectious Diseases
- Vascular Disease
- Reproductive Health
- Burns and Wound Healing
- Other
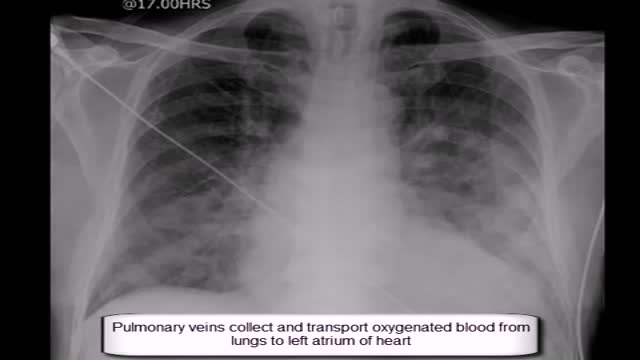
Pulmonary Artery Catheterization
Any independent vertical movement of the transducer or the patient will affect the hydrostatic column of this fluid-filled system and thus alter the pressure measurements. At some time before or after PAC insertion, the system must therefore be zeroed to ambient air pressure. The reference point for this is the midpoint of the left atrium (LA), estimated as the fourth intercostal space in the midaxillary line with the patient in the supine position. With the transducer at this height, the membrane is exposed to atmospheric pressure, and the monitor is then adjusted to zero. Calibration Once zeroed, the monitoring system must be calibrated for accuracy. Currently, most monitors perform an automated electronic calibration. Two methods are used to manually calibrate and check the system. If the catheter has not been inserted, the distal tip of the PAC is raised to a specified height above the LA. For example, raising the tip 20 cm above the LA should produce a reading of approximately 15 mm Hg if the system is working properly (1 mm Hg equals 1.36 cm H 2 O). Alternatively, pressure can be applied externally to the transducer and adjusted to a known level using a mercury or aneroid manometer. The monitor then is adjusted to read this pressure, and the system is calibrated. Dynamic tuning Central pressures are dynamic waveforms (ie, they vary from systole to diastole) and thus have a periodic frequency. To monitor these pressures accurately, the system requires an appropriate frequency response. A poorly responsive system produces inaccurate pressure readings, and differentiating waveforms (eg, PA from pulmonary capillary wedge pressure [PCWP]) can become difficult. When signal energy is lost, the pressure waveform is dampened. Common causes of this are air bubbles (which are compressible), long or compliant tubing, vessel wall impingement, intracatheter debris, transducer malfunction, and loose connections in the tubing. A qualitative test of the frequency response is performed by flicking the catheter and observing a brisk high-frequency response in the waveform. After insertion, the system can be checked by using the rapid flush test. When flushed, an appropriately responsive system shows an initial horizontal straight line with a high-pressure reading. Once the flushing is terminated, the pressure drops immediately, which is represented by a vertical line that plunges below the baseline. A brief and well-defined oscillation occurs, followed by return of the PA waveform. A dampened system will not overshoot or oscillate, and causes a delay in returning to the PA waveform.