- Physical Examination
- Surgical Examination
- Ophthalmology
- Clinical Skills
- Orthopedics
- Surgery Videos
- Laparoscopy
- Pediatrics
- Funny Videos
- Cardiothoracic Surgery
- Nursing Videos
- Plastic Surgery
- Otorhinolaryngology
- Histology and Histopathology
- Neurosurgery
- Dermatology
- Pediatric Surgery
- Urology
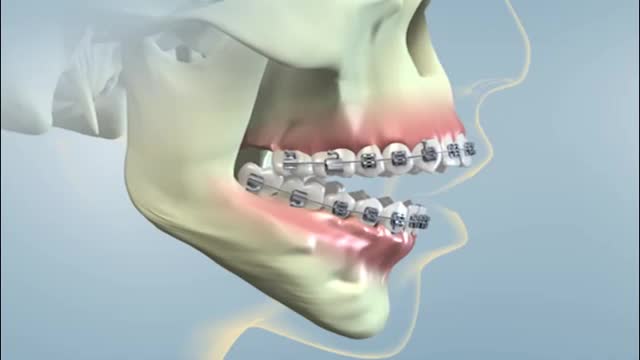
- Dentistry
- Oncology and Cancers
- Anatomy Videos
- Health and Fitness
- Radiology
- Anaesthesia
- Physical Therapy
- Pharmacology
- Interventional Radiology
- Cardiology
- Endocrinology
- Gynecology
- Emergency Medicine
- Psychiatry and Psychology
- Childbirth Videos
- General Medical Videos
- Nephrology
- Physiology
- Diet and Food Health
- Diabetes Mellitus
- Neurology
- Women Health
- Osteoporosis
- Gastroenterology
- Pulmonology
- Hematology
- Rheumatology
- Toxicology
- Nuclear Medicine
- Infectious Diseases
- Vascular Disease
- Reproductive Health
- Burns and Wound Healing
- Other
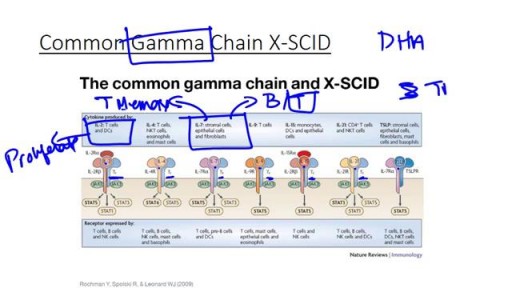
Severe combined immunodeficiency
Severe combined immunodeficiency (SCID) is a life-threatening syndrome of recurrent infections, diarrhea, dermatitis, and failure to thrive. It is the prototype of the primary immunodeficiency diseases and is caused by numerous molecular defects that lead to severe compromise in the number and function of T cells, B cells, and occasionally natural killer (NK) cells. Clinically, most patients present before age 3 months. Without intervention, SCID usually results in severe infection and death in children by age 2 years. A committee of experts, initially sponsored by the World Health Organization (WHO), meets every 2 years with the goal to classify the group of primary immunodeficiency diseases according to current understanding of the pathways that become defective in the immune system.[1] Eight classification groups have been determined, with SCID being one of the best studied. Over the past few decades, the diverse molecular genetic causes of SCID have been identified with progress from studies of the immune system.[2] SCID is considered a pediatric emergency because survival depends on expeditious stem cell reconstitution, usually by bone marrow transplantation (BMT). Appropriate diagnosis is essential because instituting proper treatment is lifesaving. Despite the heterogeneity in the pathogenesis of immune defects, common cutaneous manifestations and typical infections can provide clinical clues in diagnosing this pediatric emergency.[3] Skin manifestations were prevalent in primary immunodeficiency disorders studied in 128 pediatric patients in Kuwait; skin infections were the most prevalent findings, seen in 39 patients (30%), followed by dermatitis in 24 (19%).[4] Skin infections were significantly more prevalent in those with congenital defects in phagocyte number, function, or both, as well as in those with well-defined immunodeficiencies. Dermatitis was evident in all patients with hyper–immunoglobulin (Ig) E syndrome and Wiskott-Aldrich syndrome.[4] Erythroderma of infancy with diffuse alopecia was seen exclusively in patients with SCID disorders, and telangiectasia in patients with ataxia telangiectasia; and partial albinism with silvery gray hair was associated with Chediak-Higashi syndrome. With the advances in BMT and gene therapy, patients now have a better likelihood of developing a functional immune system in a previously lethal genetic disease. However, once an infant develops serious infections, intervention is rarely successful.