- Physical Examination
- Surgical Examination
- Ophthalmology
- Clinical Skills
- Orthopedics
- Surgery Videos
- Laparoscopy
- Pediatrics
- Funny Videos
- Cardiothoracic Surgery
- Nursing Videos
- Plastic Surgery
- Otorhinolaryngology
- Histology and Histopathology
- Neurosurgery
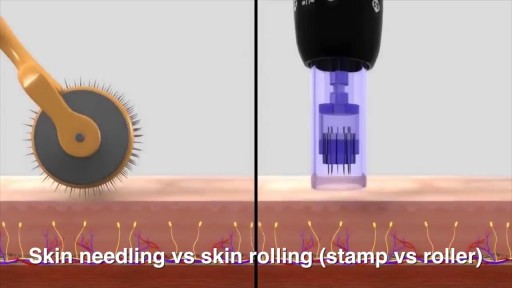
- Dermatology
- Pediatric Surgery
- Urology
- Dentistry
- Oncology and Cancers
- Anatomy Videos
- Health and Fitness
- Radiology
- Anaesthesia
- Physical Therapy
- Pharmacology
- Interventional Radiology
- Cardiology
- Endocrinology
- Gynecology
- Emergency Medicine
- Psychiatry and Psychology
- Childbirth Videos
- General Medical Videos
- Nephrology
- Physiology
- Diet and Food Health
- Diabetes Mellitus
- Neurology
- Women Health
- Osteoporosis
- Gastroenterology
- Pulmonology
- Hematology
- Rheumatology
- Toxicology
- Nuclear Medicine
- Infectious Diseases
- Vascular Disease
- Reproductive Health
- Burns and Wound Healing
- Other
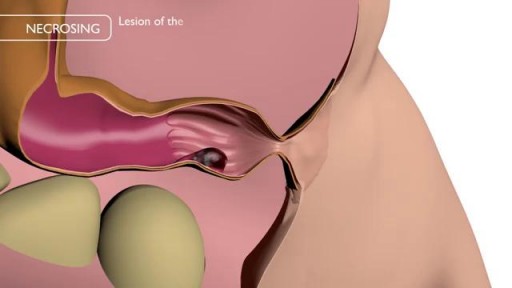
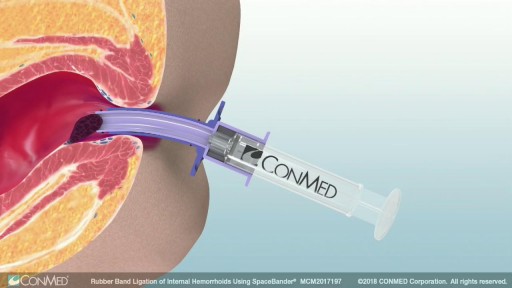
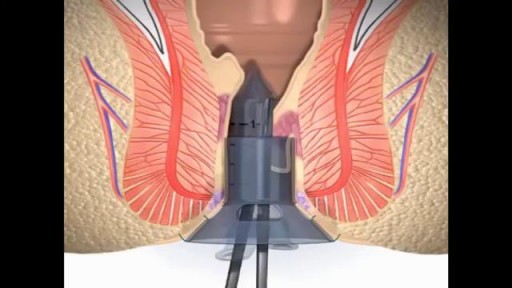
Treat HEMORRHOIDS
Most of the time, treatment for hemorrhoids involves steps that you can take on your own, such as lifestyle modifications. But sometimes medications or surgical procedures are necessary. Medications If your hemorrhoids produce only mild discomfort, your doctor may suggest over-the-counter creams, ointments, suppositories or pads. These products contain ingredients, such as witch hazel or hydrocortisone, that can relieve pain and itching, at least temporarily. Don't use an over-the-counter cream or other product for more than a week unless directed by your doctor. These products can cause side effects, such as skin rash, inflammation and skin thinning. Minimally invasive procedures If a blood clot has formed within an external hemorrhoid, your doctor can remove the clot with a simple incision, which may provide prompt relief. For persistent bleeding or painful hemorrhoids, your doctor may recommend another minimally invasive procedure. These treatments can be done in your doctor's office or other outpatient setting. Rubber band ligation. Your doctor places one or two tiny rubber bands around the base of an internal hemorrhoid to cut off its circulation. The hemorrhoid withers and falls off within a week. This procedure — called rubber band ligation — is effective for many people. Hemorrhoid banding can be uncomfortable and may cause bleeding, which might begin two to four days after the procedure but is rarely severe. Injection (sclerotherapy). In this procedure, your doctor injects a chemical solution into the hemorrhoid tissue to shrink it. While the injection causes little or no pain, it may be less effective than rubber band ligation. Coagulation (infrared, laser or bipolar). Coagulation techniques use laser or infrared light or heat. They cause small, bleeding, internal hemorrhoids to harden and shrivel. While coagulation has few side effects, it's associated with a higher rate of hemorrhoids coming back (recurrence) than is the rubber band treatment. Surgical procedures If other procedures haven't been successful or you have large hemorrhoids, your doctor may recommend a surgical procedure. Surgery can be performed on an outpatient basis or you may need to stay in the hospital overnight. Hemorrhoid removal. During a hemorrhoidectomy, your surgeon removes excessive tissue that causes bleeding. Various techniques may be used. The surgery may be done with a local anesthetic combined with sedation, a spinal anesthetic or a general anesthetic. Hemorrhoidectomy is the most effective and complete way to treat severe or recurring hemorrhoids. Complications may include temporary difficulty emptying your bladder and urinary tract infections associated with this problem. Most people experience some pain after the procedure. Medications can relieve your pain. Soaking in a warm bath also may help. Hemorrhoid stapling. This procedure, called stapled hemorrhoidectomy or stapled hemorrhoidopexy, blocks blood flow to hemorrhoidal tissue. Stapling generally involves less pain than hemorrhoidectomy and allows an earlier return to regular activities. Compared with hemorrhoidectomy, however, stapling has been associated with a greater risk of recurrence and rectal prolapse, in which part of the rectum protrudes from the anus. Talk with your doctor about what might be the best option for you.